Targeted Probe and Educate Progress Update: JJ Part A Skilled Nursing Facility (SNF)
The Centers for Medicare & Medicaid Services (CMS) Change Request 10249 (PDF, 241.88 KB) implemented the Targeted Probe & Educate (TPE) process effective October 1, 2017. The following provides JJ Probe 1 and Probe 2 TPE results statistics from January 2, 2018, to February 28, 2020.
Findings
Medical Review initiated Probe review edits for providers identified through data analysis demonstrating high risk for improper payment. Providers have been offered education throughout and upon completion of the JJ Probe 1 and Probe 2 TPE review. Current JJ Probe 1 and Probe 2 Skilled Nursing Facility (SNF) TPE Results are as follows:
Skilled Nursing Facility (SNF)
Probes Processed January 2, 2018, to February 28, 2020
| Number of Providers with Edit Effectiveness Performed Probe 1 | Providers Compliant Completed/Removed from Probe 1 Edit | Providers Non-Compliant Progressing to TPE Probe 2 | Number of Providers with Edit Effectiveness Performed Probe 2 | Providers Compliant Completed/Removed from Probe 2 Edit | Providers Non-Compliant Progressing to TPE Probe 3 | Providers Removed from Probe 1 or 2 for Other Reasons |
|---|---|---|---|---|---|---|
|
72 |
39 |
33 |
28 |
22 |
5 |
1 |
Findings by State
Palmetto GBA’s overview of results by state for providers who have had edit effectiveness performed for JJ Probe 1 and Probe 2 TPE review from January 2, 2018, to February 28, 2020.
| State | Number of Providers with Edit Effectiveness Performed Probe 1 | Providers Compliant Completed/Removed from Probe 1 Edit | Providers Non-Compliant Progressing to TPE Probe 2 | Providers Removed from Probe 1 or 2 for Other Reasons | Number of Providers with Edit Effectiveness Performed Probe 2 | Providers Compliant Completed/Removed from Probe 2 Edit | Providers Non-Compliant Progressing to TPE Probe 3 |
|---|---|---|---|---|---|---|---|
| Alabama |
5 |
0 |
5 |
1 |
5 |
2 |
2 |
| Georgia |
5 |
0 |
5 |
0 |
5 |
4 |
1 |
| Tennessee |
62 |
39 |
23 |
0 |
18 |
16 |
2 |
| State | Overall Charge Denial Rate Per State Probe 1 | Overall Charge Denial Rate Per State Probe 2 |
|---|---|---|
| Alabama |
70% |
25% |
| Georgia |
70% |
25% |
| Tennessee |
20% |
25% |
Risk Category
Risk Category is defined based on end of JJ Probe 1 provider error rates. The categories are defined as:
| Risk Category | Error Rate |
|---|---|
|
Minor |
0–20% |
|
Major |
21–100% |
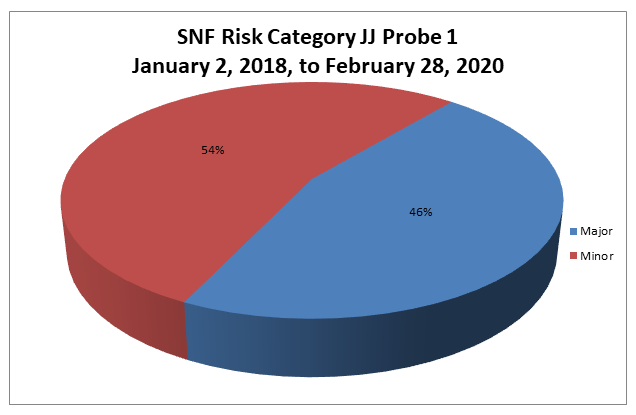
Risk Category
Risk Category is defined based on end of JJ Probe 2 provider error rates. The categories are defined as:
| Risk Category | Error Rate |
|---|---|
|
Minor |
0–20% |
|
Major |
21–100% |
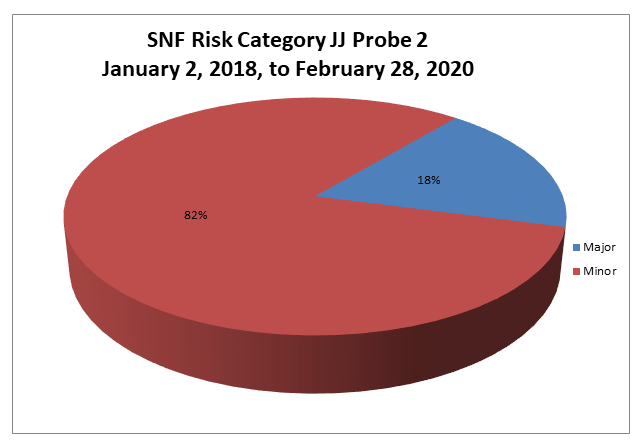
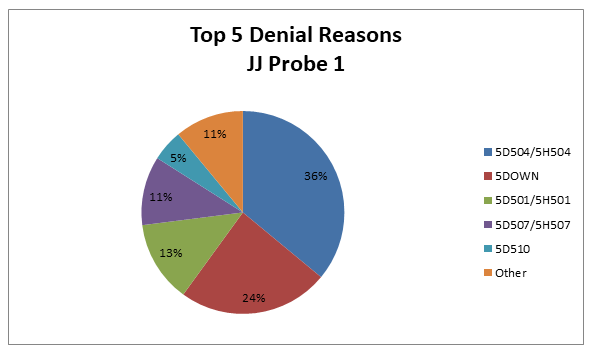
Skilled Nursing Facility
Top 5 Denial Reasons January 2, 2018, to February 28, 2020, JJ Probe 1
- 5D504/5H504 — Information Provided Does Not Support the Medical Necessity for this Service
- 5DOWN — Medical Review Downcode (Skilled Nursing Facility)
- 5D501/5H501 — Billing Error
- 5D507/5H507 — SNF MDS Is Not in the National Repository
- 5D510 — Skilled Nursing Facility Benefits Are Only Available after an Eligible Covered Hospital Stay of at Least Three Days
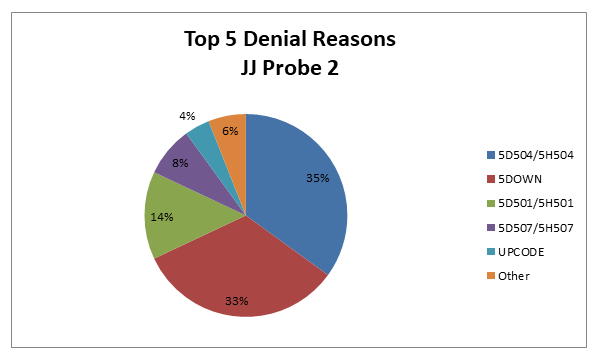
Skilled Nursing Facility
Top 5 Denial Reasons January 2, 2018, to February 28, 2020, JJ Probe 2
- 5D504/5H504 — Information Provided Does Not Support the Medical Necessity for this Service
- 5DOWN — Medical Review Downcode (Skilled Nursing Facility)
- 5D501/5H501 — Billing Error
- 5D507/5H507 — SNF MDS Is Not in the National Repository
- Upcode — Medical Review Upcode (Skilled Nursing Facility)
5D504/5H504 — Information Provided Does Not Support the Medical Necessity for this Service
Reason for Denial
The claim was fully or partially denied, as we were unable to determine medical necessity with the documentation submitted for review.
How to Avoid a Denial
- Documentation should support treatment of a condition for which the beneficiary was receiving inpatient hospital services or for a condition that arose while receiving care in a SNF for treatment of a condition for which the beneficiary was previously treated in the hospital
- Submit all documentation to support the services billed and the medical necessity of those services. Services must be medically reasonable and necessary and supported by documentation.
- Submit a copy of the qualifying hospital stay transfer/discharge summary that relates to the services provided in the Skilled Nursing Facility (SNF)
- Submit a physician certification and subsequent recertifications of the need for continuing daily skilled SNF services
- Submit the corresponding MDS for each RUG code billed. If more than one RUG code is billed, an MDS for each RUG code must be submitted for review. This may include all MDS documents from the start of care through the dates of service billed.
- Submit all documentation used to complete each MDS. This includes the documentation to cover the look back period(s) for each MDS submitted.
- Submit dated physician’s orders for all services billed, including services provided during the look back period(s). Orders for services rendered during the look back period(s) and written prior to the look back period must be submitted with the documentation.
- Any separate forms used for documentation of medication, wound care, staging of wounds, therapy minutes, weights, vital signs, intake and output, enteral feedings, nutritional consults, percentage of meals consumed, and bladder and bowel function should be submitted with the medical records
- Ensure any changes in condition or treatment that would warrant daily skilled care are documented and submitted for review. This documentation includes, but is not limited to, nurse’s notes, social worker notes, nutritional services, activity reports, progress notes, consultations, laboratory reports, X-ray reports and treatment plans.
- Documentation should include the beneficiary’s functional level and mental status, changes in treatment or medications, skilled services provided in response to physician’s orders and visits from the physician or other professional personnel
- Documentation in the form of checklists must include documentation of the beneficiary’s response to the services rendered
- Clinical documentation that furnishes a picture of the beneficiary’s care needs and response to treatment helps to establish the need for Part A services in a skilled nursing facility
5DOWN — Medical Review Down code (Skilled Nursing Facility)
Reason for Denial
The services billed were paid at a lower payment level. Based on medical review, the original Resource Utilization Group (RUG) code was downcoded. Documentation should support the data on the Minimum Data Set (MDS), paint a clear picture of the beneficiary’s medical condition and meet coverage criteria.
Under the Prospective Payment System (PPS), Medicare reimbursement rates are based on the beneficiary’s health condition and care needs. The medical documentation submitted did not support the RUG code billed. As a result, reimbursement has been adjusted to a lower payment level.
How to Avoid a Denial
- Documentation should support treatment of a condition for which the beneficiary was receiving inpatient hospital services or for a condition that arose while receiving care in a skilled nursing facility (SNF) for treatment of a condition for which the beneficiary was previously treated in the hospital
- Submit all documentation to support the services billed and the medical necessity of those services. Services must be medically reasonable and necessary and supported by documentation.
- Submit a copy of the qualifying hospital stay transfer/discharge summary that relates to the services provided in the skilled nursing facility (SNF)
- Submit a physician’s certification and subsequent recertifications of the need for continuing daily skilled SNF services
- Submit the corresponding Minimum Data Set (MDS) for each RUG code billed. If more than one RUG code is billed, an MDS for each RUG code must be submitted for review. This may include all MDS documents from the start of care through the dates of service billed.
- Submit all documentation used to complete each MDS. This includes the documentation to cover relevant look back periods for each MDS submitted.
- Submit dated physician’s orders for all services billed, including services provided during the look back period(s). If orders for services rendered during the look back period(s) was/were written prior to the look back period, they must be submitted with the documentation.
- Include any separate forms used for documentation of medication, wound care, staging of wounds, therapy minutes, weights, vital signs, intake and output, enteral feedings, nutritional consults, percentage of meals consumed and bladder and bowel function with the submitted records
- Ensure any changes in condition or treatment that would warrant daily skilled care are documented and submitted for review. This documentation includes, but is not limited to, nurses’ notes, social worker notes, nutritional services, activity reports, progress notes, consultations, laboratory reports, X-ray reports and treatment plans.
- Documentation should include the beneficiary’s functional level and mental status, changes in treatment or medications, the skilled services provided in response to physician’s orders and visits from the physician or other professional personnel
- Documentation in the form of checklists must include documentation of the beneficiary’s response to the services rendered
- Clinical documentation that furnishes a picture of the beneficiary’s care needs and response to treatment helps to establish the need for Part A services in a SNF
Therapy-specific information and hints, if applicable:
- The initial therapy evaluation must be performed in the SNF and the actual minutes used for this evaluation cannot be included in the minutes of therapy on the MDS
- Minutes recorded on the MDS must be the actual minutes of therapy rendered and must be supported by the therapist’s documentation
- The initial therapy evaluation must reflect the resident’s ability to retain instructions
- When therapy services are provided, there must be an expectation of improvement within a reasonable period of time
- Repetitious therapy exercises that could be performed by aides and/or nursing personnel are not considered skilled services
- Therapy is not required in a situation where a beneficiary suffers a transient and easily reversible loss or reduction in function, which could reasonably be expected to improve spontaneously as the beneficiary gradually resumes normal activities
- If speech-language pathology (SLP) services are rendered for the treatment of dysphagia, submit all supporting documentation to establish the medical necessity of the billed services. This may include, but is not limited to, physician’s notes and test results. An example of tests for treatment of dysphagia is modified barium swallow (MBS) and/or a fiberoptic endoscopic examination of swallowing (FEES).
- Specific documentation related to therapy services must be submitted for review. This includes, but is not limited to, the following:
- Physician’s orders for therapy services
- Documentation to establish that the therapy services are of a complexity that requires the skills of a licensed therapist
- A written therapy plan of treatment established by the physician after consultation with the therapist. The physician must sign this plan of treatment.
- Documentation to establish the medical necessary of the therapy services as it relates to the illness/injury of the beneficiary
- Short term and long-term goals (measurable)
- Actual minutes of therapy rendered as documented on a log/grid or in the clinical documentation
- Progress notes and documentation of treatment modalities rendered
- Level of function just prior to the spell of illness
- Functional decline
- Current level of function
- Documentation must clearly establish that occupational therapy (OT) and physical therapy (PT) are not duplicating services
- If the beneficiary is readmitted to the facility and therapy is continued, a new evaluation must be performed and submitted for review
5D501 — 5H501 — Billing Error
Reason for Denial
The service(s) billed (was/were) not covered because, according to the documentation in the medical record, the SNF has made a billing error. Therefore, no Medicare payment will be made. The SNF may not charge the beneficiary for service(s) that (was/were) billed in error.
How to Avoid a Denial
Ensure that all charges for accuracy/timeliness are correct prior to submitting the final bill to Medicare. Check to ensure that all documentation submitted in response to the ADR corresponds to the service(s) rendered and the dates of service(s) billed.
5D507/5H507 — SNF MDS Is Not in the National Repository
Reason for Denial
The services billed were not covered because the Minimum Data Set (MDS) cannot be found in the National Repository.
How to Avoid a Denial
- Ensure that the MDS has been entered into the National Repository prior to submitting request for payment to Medicare
- Check all bills for accuracy and ensure that the MDS clinical assessment includes data for all covered days associated with the billing period
5D510 – Skilled Nursing Facility Benefits Are Only Available after an Eligible Covered Hospital Stay of at Least Three Days
Reason for Denial
The service(s) billed [was/were] not covered by Medicare, as the documentation submitted did not meet the three consecutive calendar hospital stay requirement.
How to Avoid a Denial
The three consecutive calendar day stay requirement can be met by stays totaling three consecutive days in one or more hospitals. In determining whether the requirement has been met, the day of admission but not the day of discharge is counted as a hospital inpatient day. In addition, the qualifying hospital stay must be medically necessary.
UPCODE — Medical Review Upcode (Skilled Nursing Facility)
Reason for Denial
The services billed were paid at a higher payment level. Based on medical review, the original Resource Utilization Group (RUG) code was up coded. Documentation should support the data on the Minimum Data Set (MDS), paint a clear picture of the beneficiary’s medical condition, and meet coverage criteria.
Under the Prospective Payment System (PPS), Medicare reimbursement rates are based on the beneficiary’s health condition and care needs. The medical documentation submitted did not support the RUG code billed. As a result, reimbursement has been adjusted to a higher payment level.
How to Avoid a Denial
- Documentation should support treatment of a condition for which the beneficiary was receiving inpatient hospital services or for a condition that arose while receiving care in a skilled nursing facility (SNF) for treatment of a condition for which the beneficiary was previously treated in the hospital
- Submit all documentation to support the services billed and the medical necessity of those services. Services must be medically reasonable and necessary and supported by documentation.
- Submit a copy of the qualifying hospital stay transfer/discharge summary that relates to the services provided in the skilled nursing facility (SNF)
- Submit a physician’s certification and subsequent recertifications of the need for continuing daily skilled SNF services
- Submit the corresponding Minimum Data Set (MDS) for each RUG code billed. If more than one RUG code is billed, an MDS for each RUG code must be submitted for review. This may include all MDS from the start of care through the dates of service billed.
- Submit all documentation used to complete each MDS. This includes the documentation to cover relevant look back periods for each MDS submitted.
- Submit dated physician’s orders for all services billed, including services provided during the look back period(s). If orders for services rendered during the look back period(s) were written prior to the look back period, they must be submitted with the documentation.
- Include any separate forms used for documentation of medication, wound care, staging of wounds, therapy minutes, weights, vital signs, intake and output, enteral feedings, nutritional consults, percentage of meals consumed, bladder and bowel function with the submitted records
- Ensure any changes in condition or treatment that would warrant daily skilled care are documented and submitted for review. This documentation includes, but is not limited to, nurses’ notes, social worker notes, nutritional services, activity reports, progress notes, consultations, laboratory and X-ray reports, and treatment plans.
- Documentation should include the beneficiary’s functional level and mental status, changes in treatment or medications, the skilled services provided in response to physician’s orders, and visits from the physician or other professional personnel
- Documentation in the form of checklists must include documentation of the beneficiary’s response to the services rendered
- Clinical documentation that furnishes a picture of the beneficiary’s care needs and response to treatment helps to establish the need for Part A services in a SNF
Therapy-specific information and hints, if applicable:
- The initial therapy evaluation must be performed in the SNF and the actual minutes used for this evaluation cannot be included in the minutes of therapy on the MDS
- Minutes recorded on the MDS must be the actual minutes of therapy rendered and must be supported by the therapist’s documentation
- The initial therapy evaluation must reflect the resident’s ability to retain instructions
- When therapy services are provided, there must be an expectation of improvement within a reasonable period of time
- Repetitious therapy exercises that could be performed by aides and/or nursing personnel are not considered skilled services
- Therapy is not required in a situation where a beneficiary suffers a transient and easily reversible loss or reduction in function, which could reasonably be expected to improve spontaneously as the beneficiary gradually resumes normal activities
- If speech-language pathology (SLP) services are rendered for the treatment of dysphagia, submit all supporting documentation to establish the medical necessity of the billed services. This may include, but is not limited to, physician’s notes and test results, for example, a modified barium swallow (MBS) and/or a fiberoptic endoscopic examination of swallowing (FEES).
- Specific documentation related to therapy services must be submitted for review. This includes, but is not limited to, the following:
- Physician’s orders for therapy services
- Documentation to establish that the therapy services are of a complexity that requires the skills of a licensed therapist
- A written therapy plan of treatment established by the physician after consultation with the therapist. The physician must sign this plan of treatment.
- Documentation to establish the medical necessary of the therapy services as it relates to the illness/injury of the beneficiary
- Short term and long-term goals (measurable)
- Actual minutes of therapy rendered as documented on a log/grid or in the clinical documentation
- Progress notes and documentation of treatment modalities rendered
- Level of function just prior to the spell of illness
- Functional decline
- Current level of function
- Documentation must clearly establish that occupational therapy (OT) and physical therapy (PT) are not duplicating services
- If the beneficiary is readmitted to the facility and therapy is continued, a new evaluation must be performed and submitted for review
Education
Providers are offered an individualized education session where each claim denial will be discussed, and any questions will be answered. Palmetto GBA offers a variety of methods for provider education such as webinar sessions, web-based presentations or teleconferences. Other education methods may also be available.
Next Steps
Providers found to be non-compliant (major risk category/denial rate of 21–100%) at the completion of TPE Probe 1 will advance to Probe 2 and Providers found to be non-compliant (major risk category/denial rate of 21–100%) at the completion of TPE Probe 2 will advance to Probe 3 of TPE at least 45 days from completion of the 1:1 post probe education call date. Palmetto GBA offers education at any time for providers. Providers do not have to be identified for TPE to request education.
References
- CMS Targeted Probe and Educate (TPE) web page
- Change Request 10249 (PDF, 241.88 KB)