Targeted Probe and Educate Progress Update: JJ Part A Infliximab J1745
The Centers for Medicare & Medicaid Services (CMS) Change Request 10249 (PDF, 241.88 KB) implemented the Targeted Probe and Educate (TPE) process effective October 1, 2017. The following provides JJ Probe 1 TPE results statistics from January 2, 2018, to February 28, 2020.
Findings
Medical Review initiated Probe review edits for providers identified through data analysis demonstrating high risk for improper payment. Providers have been offered education throughout and upon completion of the Probe 1 TPE review. Current JJ Part A Probe 1 Infliximab J1745 TPE Results are as follows:
Infliximab J1745
Probes Processed January 2, 2018, to February 28, 2020
| Number of Providers with Edit Effectiveness Performed Probe 1 | Providers Compliant Completed/Removed After Probe 1 Edits | Providers Non-Compliant Progressing to TPE Probe 2 | Providers Removed from Probe 1 for Other Reasons |
|---|---|---|---|
|
16 |
12 |
4 |
0 |
Findings by State
Palmetto GBA’s overview of results by state for providers who have had edit effectiveness performed for JJ Probe 1 TPE review from January 2, 2018, to February 28, 2020.
| State | Number of Providers with Edit Effectiveness Performed Probe 1 | Providers Compliant Completed/Removed After Probe 1 | Providers Non-Compliant Progressing to TPE Probe 2 | Providers Removed After Probe 1 for Other Reasons | Overall Charge Denial Rate Per State Probe 1 |
|---|---|---|---|---|---|
| Alabama |
4 |
4 |
0 |
0 |
11% |
| Georgia |
9 |
5 |
4 |
0 |
22% |
| Tennessee |
3 |
3 |
0 |
0 |
7% |
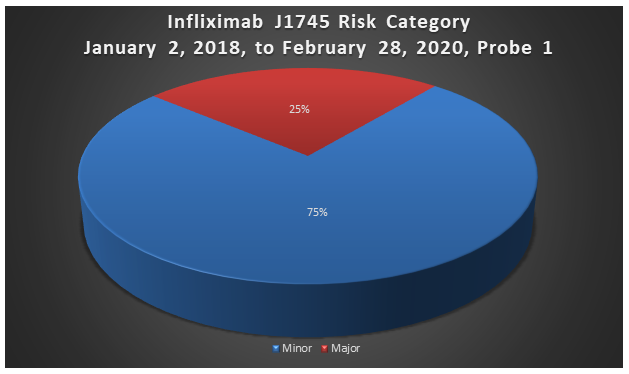
Risk Category
Risk Category is defined based on end of JJ Probe 1 provider error rates. The categories are defined as:
| Risk Category | Error Rate |
|---|---|
|
Minor |
0–20% |
|
Major |
21–100% |
Infliximab J1745
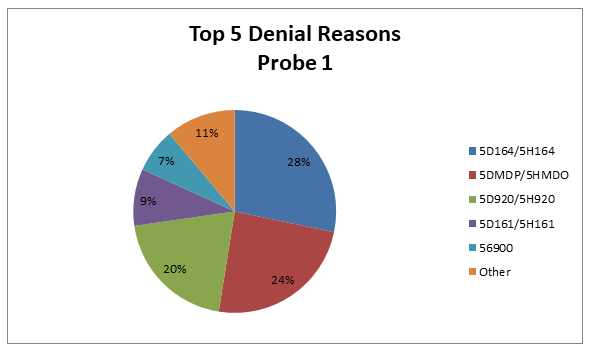
Top 5 Denial Reasons January 2, 2018, to February 28, 2020, JJ Probe 1
- 5D164/5H164 — No Documentation of Medical Necessity
- 5DMDP/5HMDP — Dependent Services Denied (Qualifying Service Denied Medically)
- 5D920/5H920 — The Recommended Protocol Was Not Ordered and/or Followed
- 5D161/5H161 — No Physician’s Orders
- 56900 — Auto Deny — Requested Records Not Submitted Timely
5D164/5H164 — No Documentation of Medical Necessity
Reason for Denial
This claim was fully or partially denied because the documentation submitted for review does not support the medical necessity of some of the services billed.
How to Avoid a Denial
- Submit all documentation related to the service(s) billed which support the medical necessity of the service(s)
- A legible signature is required on all documentation necessary to support orders and medical necessity
- Use the most appropriate ICD-10-CM codes to identify the beneficiary’s medical diagnosis
5DMDP/5HMDP – Dependent Services Denied (Qualifying Service Denied Medically)
Reason for Denial
The dependent service(s) will not be covered if the qualifying surgery has been denied. For example, the surgical procedure was denied as documentation did not support medical necessity; therefore, all other charges cannot be allowed and will be denied as dependent to the medical denial of the qualifying service(s).
How to Avoid a Denial
Documentation that may be helpful to avoid future denials for this reason may include, but is not limited to, the following:
- All documentation to support orders, documentation of services rendered and documentation of medical necessity for the qualifying service(s) for the date(s) billed
5D920/5H920 — The Recommended Protocol was not Ordered and/or Followed
Reason for Denial
Medicare cannot pay for this service because one or more requirements for coverage was/were not met.
How to Avoid a Denial
Documentation that may be helpful to avoid future denials for this reason may include, but are not limited to, the following:
- Clear physician’s order with indication of need, dose, frequency and route
- Date and time of associated chemotherapy, as applicable
- Relevant history and physical and/or progress notes
- Clear indication of the diagnosis
- Clinical signs and symptoms
- Prior treatment and response, as applicable
- Stage of treatment, as applicable
- Documentation of administration
5D161/5H161 — No Physician’s Orders
Reason for Denial
This claim was fully or partially denied because there were no physician’s orders submitted for review for all or some of the services billed.
How to Avoid a Denial
- A physician’s order should be submitted for review with the request for copies of medical records
- A legible signature is required on all documentation necessary to support orders and medical necessity
- The copy of the order should be legible and dated
- Make sure any orders submitted for review are for the date(s) of service billed
56900 — Auto Deny — Requested Records Not Submitted Timely
Reason for Denial
The services billed were not covered because the claim was not submitted or not submitted timely in response to an Additional Documentation Request (ADR). The provider has 45 days from the date the ADR was generated to respond with medical records. In accordance with CMS instruction, a medical determination will be made by Palmetto GBA if the documentation is not received within the 45-day timeframe based on the available medical documentation. If the claim is denied, payment will be denied, or an overpayment will be collected.
How to Avoid a Denial
- Be aware of the ADR date and the need to submit medical records within 45 days of the ADR date
- Submit the medical records as soon as the ADR is received
- Monitor the status of your claims in Direct Data Entry (DDE) and begin gathering the medical records as soon as the claim goes to the status/location of SB6001
- Return the medical records to the address on the ADR. Be sure to include the appropriate mail code or station number. This ensures that your responses are promptly routed to the Medical Review Department.
- Gather all the information needed for the claim and submit it all at one time
- Attach a copy of the ADR request to each individual claim
- If responding to multiple ADRs, separate each response and attach a copy of the ADR to each individual set of medical records. Make sure each set of medical records is bound securely with one staple in the upper left corner or a rubber band to ensure that no documentation is detached or lost. Do not use paper clips.
- Do not mail packages C.O.D.; we cannot accept them
Education
Providers are offered an individualized education session where each claim denial will be discussed, and any questions will be answered. Palmetto GBA offers a variety of methods for provider education such as webinar sessions, web-based presentations or teleconferences. Other education methods may also be available.
Next Steps
Providers found to be non-compliant (major risk category/denial rate of 21–100%) at the completion of TPE Probe 1 will advance to Probe 2 at least 45 days from completion of the 1:1 post probe education call date. Palmetto GBA offers education at any time for providers. Providers do not have to be identified for TPE to request education. Palmetto GBA offers education at any time for providers. Providers do not have to be identified for TPE to request education.
References
- CMS Targeted Probe and Educate (TPE) web page
- Change Request 10249 (PDF, 241.88 KB)