Pre-Payment Review Results for Intensity Modulated Radiotherapy for October Through December 2022
Cumulative Results
|
Number of Providers with Edit Effectiveness |
Providers Compliant Completed/Removed After Probe |
Providers Non-Compliant Progressing to Subsequent Probe |
Providers Non-Compliant/Removed for Other Reason |
|---|---|---|---|
|
3 |
3 |
0 |
0 |
|
Number of Claims with Edit Effectiveness |
Number of Claims Denied |
Overall Claim Denial Rate |
Total Dollars Reviewed |
Total Dollars Denied |
Overall Charge Denial Rate |
|---|---|---|---|---|---|
|
120 |
34 |
28% |
$463,724.94 |
$35,911.12 |
8% |
Probe One Findings
|
State |
Number of Providers with Edit Effectiveness |
Providers Compliant Completed/Removed After Probe |
Providers Non-Compliant Progressing to Subsequent Probe |
Providers Non-Compliant/Removed for Other Reason |
|---|---|---|---|---|
|
N.C. |
2 |
2 |
0 |
0 |
|
S.C. |
0 |
0 |
0 |
0 |
|
Va. |
1 |
1 |
0 |
0 |
|
W.Va. |
0 |
0 |
0 |
0 |
|
State |
Number of Claims with Edit Effectiveness |
Number of Claims Denied |
Overall Claim Denial Rate |
Total Dollars Reviewed |
Total Dollars Denied |
Overall Charge Denial Rate |
|---|---|---|---|---|---|---|
|
N.C. |
80 |
4 |
5% |
$228,677.40 |
$3,853.42 |
2% |
|
S.C. |
0 |
0 |
0% |
$0 |
$0 |
0% |
|
Va. |
40 |
30 |
75% |
$235,047.54 |
$32,057.70 |
14% |
|
W.Va. |
0 |
0 |
0% |
$0 |
$0 |
0% |
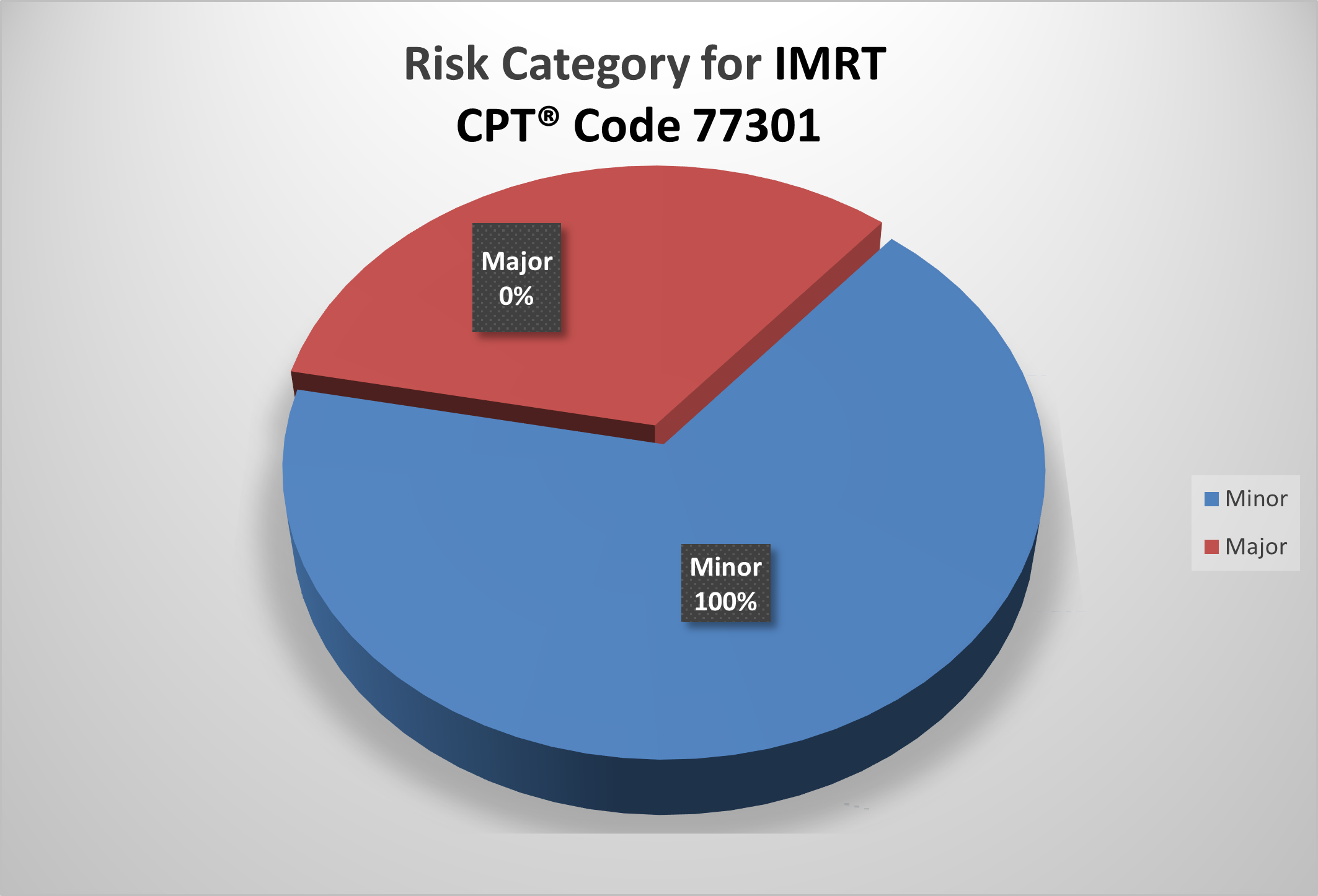
Risk Category
The categories for Current Procedural Terminology (CPT®) code 77301 for IMRT are defined as:
| Risk Category | Error Rate |
|---|---|
| Minor | 0–20% |
| Major | 21–100% |
Top Denial Reasons
|
Percent of Total Denials |
Denial Code |
Denial Description |
Number of Occurrences |
|---|---|---|---|
|
60% |
5D164/5H164 |
No Documentation of Medical Necessity |
3 |
|
40% |
5D920/5H920 |
The Recommended Protocol Was Not Ordered and/or Followed |
2 |
Denial Reasons and Recommendations
5D164/5H164 — No Documentation of Medical Necessity
Reason for Denial
This claim was denied because the documentation submitted does not support the medical necessity of the service reviewed. The records did not contain any covered condition/indication, symptomology or diagnostic results that would support the service was reasonable and necessary for the treatment of the beneficiary.
How to Avoid This Denial
- Submit all documentation related to the services billed which support the medical necessity of the services. Documentation should support:
- A covered indication or condition for the service billed
- A physician/NPP is managing the care of the covered indication or condition
- Any medical history that supports a need for the service
- Any diagnostic results or symptomology that supports a need for the service
- A legible physician or nonphysician provider (NPP) signature is required on all documentation necessary to support medical necessity
- Use the most appropriate ICD-10-CM codes to identify the beneficiary’s medical diagnosis
More Information
- 42 Code of Federal Regulations (CFR) — Section 411.15
- Social Security Act (SSA) — Section 1862(a)(1)(A)
- CMS.gov
- PalmettoGBA.com — Medicare Medical Records: Signature Requirements, Acceptable and Unacceptable Practices
5D920/5H920 — The Recommended Protocol Was Not Ordered and/or Followed
Reason for Denial
Medicare cannot pay for this service because one or more requirements for coverage were not met.
How to Avoid This Denial
Documentation that may be helpful to avoid future denials for this reason may include, but are not limited to, the following:
For Drugs and Biologicals
- Clear physician’s order with indication of need, dose, frequency, administration time and route
- Date and time of associated chemotherapy, as applicable
- Relevant medical history documented prior to the date of service (DOS) and signed by the physician or appropriate NPP to include, but not limited to:
- Clear indication of the diagnosis and need for the related service(s)
- Clinical signs and symptoms
- Prior treatment and response as applicable
- Stage of treatment as applicable
- Documentation of administration and signed by the person providing the service
- Ensure the service was provided per the coverage guidelines for the service
For Outpatient Therapy
- Clear physician’s order with indication of specific skilled service, frequency and duration
- Relevant medical history documented prior to the DOS and signed by the physician or appropriate non-physician provider to include, but not limited to:
- Clear indication of the diagnosis and need for the related therapy services
- Documentation related to the therapy services to include beneficiary's functional level, treatment plan, short- and long-term goals, beneficiary's response to therapy services, treatment and progress notes
- Prior treatment and response as applicable
- Ensure the service was provided per the coverage guidelines for the service
For IMRT
- Clear physician/radiation oncologist orders for radiation treatment course, including specific anatomical target volumes, treatment technique, current dosage, type of radiation measuring and monitoring devices to be used and treatment fields
- Relevant medical history documented prior to the DOS and signed by the physician/radiation oncologist or appropriate nonphysician provider to include:
- Clear indication of the diagnosis being treated and medical necessity of the services
- Supporting reports such as dosimetry, physicist, simulation, oncology and radiology
- Documentation of design and construction of Multi-Leaf Collinator
- Detailed itemized bill and supporting documentation of all billed services
- Documentation of treatment plan, including goals, treatment notes, specific dose constraints for the target and administration
- Ensure the service was provided per the coverage guidelines for the service
More Information
- CMS.gov
Education
Palmetto GBA offers providers selected for TPE an individualized education session to discuss each claim denial. This is an opportunity to learn how to identify and correct claim errors. A variety of education methods are offered such as webinar sessions, web-based presentations, or teleconferences. Other education methods may also be available. Providers do not have to be selected for TPE to request education. If education is desired, please complete the Education Request form (PDF).
Next Steps
Providers found to be non-compliant (major risk category/denial rate of 21–100 percent) at the completion of TPE Probe 1 will advance to Probe 2, and providers found to be non-compliant (major risk category/denial rate of 21–100 percent) at the completion of TPE Probe 2 will advance to Probe 3 of TPE after at least 45 days from completing the 1:1 post-probe education call date.