Prior Authorization of Repetitive Scheduled Non-Emergent Ambulance Transports
Prior authorization helps ambulance suppliers ensure that their services comply with applicable Medicare coverage, coding, and payment rules before services are rendered and before claims are submitted for payment.
Prior authorization does not create new clinical documentation requirements. Instead, it requires the same information necessary to support Medicare payment, just earlier in the process. Prior authorization allows providers and suppliers to address issues with claims prior to rendering services and submitting claims for payment, which has the potential to reduce appeals in the case of disputed claims.
Ambulance HCPCS Codes
The following ambulance HCPCS codes are subject to prior authorization under the model:
- A0426 — Ambulance service, Advanced Life Support (ALS), non-emergency transport, Level 1
- A0428 — Ambulance service, Basic Life Support (BLS), non-emergency transport
The mileage code, A0425, will be handled as an associated procedure for prior authorization processing and should always be billed in conjunction with the transport code. Prior authorization is not needed for A0425.
Number of Trips
An affirmative prior authorization decision affirms a specified number of trips within a specific amount of time.
- The prior authorization decision, justified by documentation of the beneficiary’s condition, may affirm up to 40 round trips (which equates to 80 trips) per prior authorization request in a 60-day period
- An affirmative prior authorization decision may affirm less than 40 round trips, or affirm a request that seeks to provide a specified number of transports (40 round trips or less) in less than a 60-day period
- An affirmative decision can be for all or part of the requested number of trips
Transports exceeding 40 round trips (or 80 one-way trips) in a 60-day period require an additional prior authorization request.
Submitting a Request
Suppliers should complete the Prior Authorization Form for their jurisdiction.
- JM Prior Authorization Form (PDF)
- JJ Prior Authorization Form (PDF)
The Prior Authorization Request needs to contain the following:
- The beneficiary's name, Medicare number, and date of birth (name and date need to match what is in the system)
- The certifying physician's name, National Provider Identifier (NPI), PTAN* and address
- The ambulance supplier's name, NPI, PTAN and address
- The requestor's name and telephone number
- Procedure code
- Submission date
- Start of 60-day period
- State where the ambulance is garaged
- Indicate if the request is an initial or resubmission review
*Not mandatory
The Request must be legible and include:
- Physician Certification Statement
- The regulations governing PCS requirements for repetitive, scheduled, non-emergency ambulance services are specified at 42 CFR §410.40(d)(2)
- Number of transports requested
- Documentation from the medical record to support the medical necessity of repetitive scheduled non-emergent ambulance transport
- Information on the origin and destination of the transports
- Any other relevant document as deemed necessary by the Medicare contractor to process the prior authorization
The documentation requirements for Medicare coverage have not changed. The same information is necessary to support Medicare payment, just earlier in the process. We strongly recommend the article "Documentation Tips for Medics: Paint the Picture," which outlines the medical documentation requirements.
Suppliers have four options for submitting prior authorization requests to the A/B MACs:
- U.S. Mail;
- Fax;
- Electronic submission of medical documentation (esMD); or
- eServices
For more information about esMD, visit the CMS website.
Review Timeframes: Initial Requests
- Palmetto GBA makes every effort to review requests and postmark decision letters within seven (7) calendar days
Subsequent Requests
- Palmetto GBA makes every effort to review requests and postmark decision letters within seven (7) calendar days
Letters are sent that communicate the decision made on the submitted prior authorization request.
| Decision Letter | Description |
|---|---|
| Anything other than affirmed or non-affirmed decisions |
|
| Affirmed or non-affirmed decisions |
|
| Detailed letter | Description |
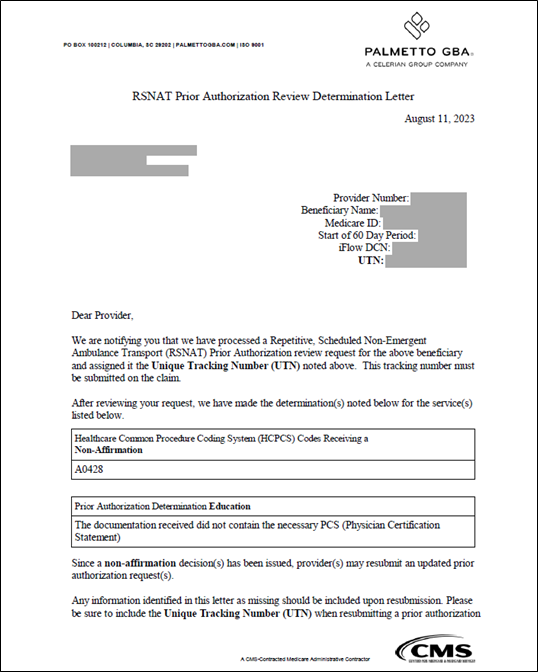
| Non-affirmed decisions made medical review |
|
Examples
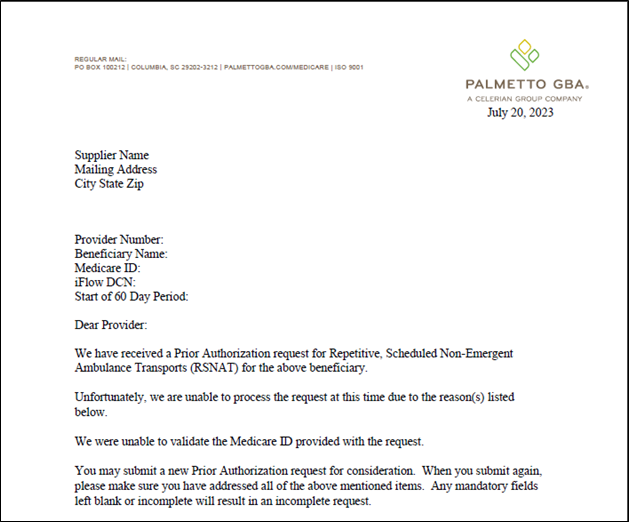
An example of an "Incomplete Prior Authorization" request. This is what the letter looks like for anything other than affirmations or non-affirmations.
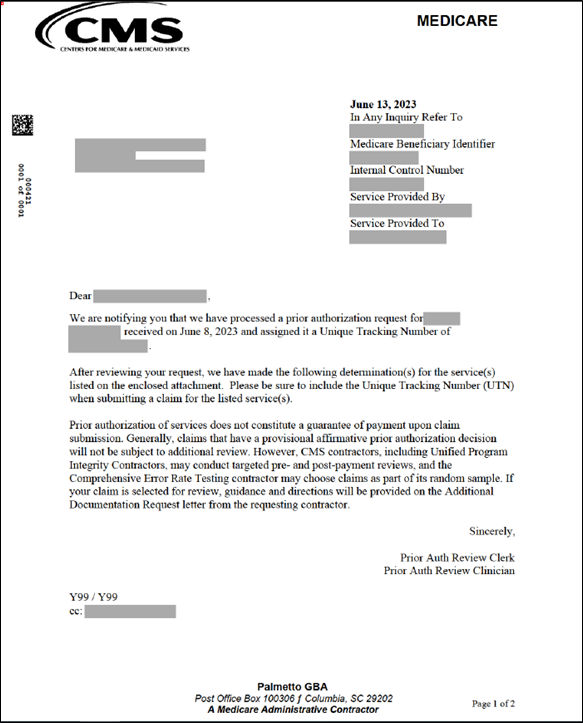
An example of a "Decision Letter" affirming the requested transports.
An example of the "Reason Field" contains the decision on the request. The decision can be affirmed or non-affirmed.
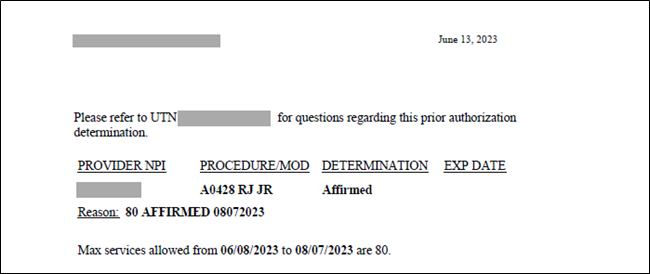
Example 1: Affirmed: REASON: 80
Example 2: Non-Affirmed: REASON: AMB6Z
For non-affirmed determinations, the code provided in the letter (i.e., AMB6Z) can be found on the crosswalk. The crosswalk is a table that lists the non-affirmation reason codes and their descriptions. These are the reasons why the request is not fully approved or affirmed.
For affirmed determinations, the number of transports approved will be listed in the "Reason" field.
Here are the Non-Affirmed Code Crosswalk: Prior Authorization Request listings.
Example: the non-affirmed reason that comes back on the decision letter is "AMB4H." By looking at the crosswalk, it can be determined that The PCS (Physician Certification Statement) received does not indicate why transportation by any other means is contraindicated. (Per 42 C.F.R. § 410.40(e)(2)).
The Unique Tracking Number (UTN) for the request is also included on these decision letters.
Additional Detail Letter Example
UTN
Each completed prior authorization request is assigned a 14 byte unique tracking number (UTN). This number will be used when submitting claims related to the prior authorization request and is included on the decision letter.
Resubmitting a Prior Authorization Request
- The supplier should review the decision letter that was provided, as well as the detail letter if one was received
- The supplier should make whatever modifications are needed to the prior authorization package and follow the submission procedures
- If this is the first time you have requested prior authorization for this 60-day period, indicate on the prior authorization request form that it is an Initial submission to preserve the seven (7) calendar day decision letter indicated the request was incomplete, indicate on the prior authorization request form that it is an Initial submission to preserve the seven (7)-day review time frame
- If a prior authorization request has been previously non-affirmed for the 60 day period, indicate Resubmission on the request form
- The A/B MAC will provide notification of the decision through a detailed decision letter postmarked within seven (7) calendar days of the review(s) to all parties affected for resubmissions
- Unlimited resubmissions are allowed for non-affirmed prior authorization requests
- These requests are not considered appeals
Submitting a Claim
- Deliver the service to beneficiary
- Have all documentation available should it be requested
- Submit the claim with the UTN on the claim
- The submission of the prior authorized transport claim is to have the 14 byte unique tracking number that is located on the decision letter. For submission of a claim on a 1500 Claim Form, the unique tracking number is submitted in the first 14 positions in item 23. All other data submitted in item 23 must begin in position 15. For submission of electronic claims, the unique tracking number must be submitted in the 2300 — Claim Information loop in the Prior Authorization reference (REF) segment where REF01 = "G1" qualifier and REF02 = UTN. A UTN submitted in this loop applies to the entire claim unless it is overridden in the REF segment in the 2400 Service Line Loop.
- If all requirements are met the claim will be paid
- The prior authorization model has specific parameters for pre-payment review; however other contractors (CERT, ZPICs, etc.) may have parameters outside of the prior authorization model that will suspend the same claim for another type of review. If your claim is selected for review, guidance and directions will be provided on the additional documentation request letter from Palmetto GBA.
Appeals
This prior authorization model does not include a separate appeal process for non-affirmative prior authorization request decisions.
However, a non-affirmative prior authorization request decision does not prevent the supplier from submitting a claim. Such a submission of a claim and resulting denial by the A/B MAC would constitute an initial determination that would make the appeals process available for disputes by Medicare beneficiaries and suppliers.
References