Targeted Probe and Educate Progress Update: JJ E/M 99232-99233: Subsequent Hospital Care
The Centers for Medicare & Medicaid Services (CMS) Change Request 10249 (PDF, 241.88 KB) implemented the Targeted Probe and Educate (TPE) process, effective October 1, 2017. The following provides JJ TPE Probe results statistics from January 2, 2018, to February 28, 2020.
Findings
Medical Review initiated Probe review edits for providers identified through data analysis demonstrating high risk for improper payment. Providers have been offered education throughout and upon completion of the Probe TPE review. Current JJ Probes 1 and 2, Part B E/M 99232–99233 Subsequent Hospital Care TPE results are as follows:
E/M 99232–99233 — Subsequent Hospital Care
Probes Processed January 2, 2018, to February 28, 2020
| Number of Providers with Edit Effectiveness Performed from January 2, 2018 – February 28, 2020, Probe 1 | Providers Compliant Completed/Removed After Probe 1 Edits | Providers Non-Compliant Progressing to TPE Probe 2 | Providers Non-Compliant/Removed for Other Reason |
|---|---|---|---|
|
285 |
96 |
189 |
1 |
| Number of Providers with Edit Effectiveness Performed from January 2, 2018 – February 28, 2020, Probe 2 | Providers Compliant Completed/Removed After Probe 2 Edits | Providers Non-Compliant Progressing to TPE Probe 3 | Providers Non-Compliant/Removed for Other Reason |
|---|---|---|---|
|
24 |
20 |
4 |
1 |
Findings by State
Palmetto GBA’s overview of results by state, for providers who have had edit effectiveness performed, for Probe 1 TPE review from January 2, 2018, to February 28, 2020.
| State | Number of Providers with Edit Effectiveness Performed from January 2, 2018 – February 28, 2020 Probe 1 | Providers Compliant Completed/Removed After Probe 1 | Providers Non-Compliant Progressing to TPE Probe 2 | Providers Non-Compliant/Removed for Other Reason | Overall Charge Denial Rate Per State |
|---|---|---|---|---|---|
| Alabama |
19 |
4 |
15 |
0 |
42% |
| Georgia |
139 |
30 |
109 |
0 |
32% |
| Tennessee |
127 |
62 |
65 |
1 |
16% |
| State | Number of Providers with Edit Effectiveness Performed from January 2, 2018 – February 28, 2020 Probe 2 | Providers Compliant Completed/Removed After Probe 2 | Providers Non-Compliant Progressing to TPE Probe 3 | Providers Non-Compliant/Removed for Other Reason | Overall Charge Denial Rate Per State |
|---|---|---|---|---|---|
| Alabama |
4 |
3 |
1 |
0 |
5% |
| Georgia |
19 |
17 |
2 |
0 |
8% |
| Tennessee |
1 |
0 |
1 |
0 |
12% |
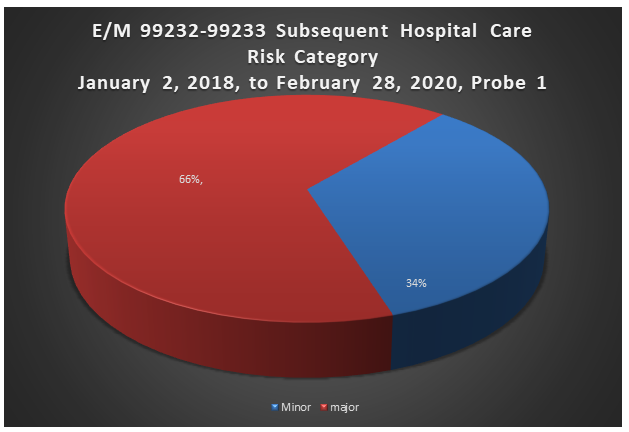
Risk Category
Risk Category is defined based on end of Probe 1 provider error rates. The categories are defined as:
| Risk Category | Error Rate |
|---|---|
|
Minor |
0–20% |
|
Major |
21–100% |
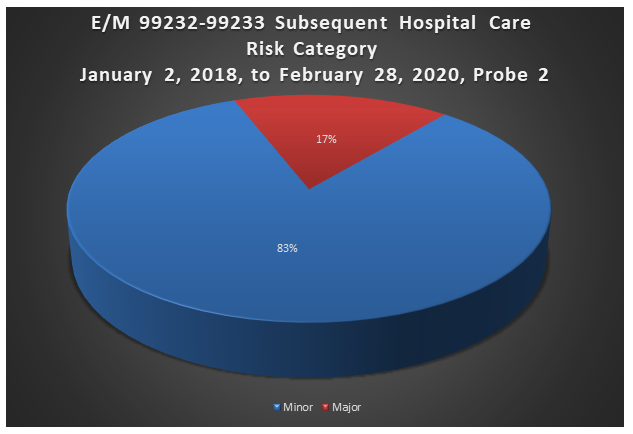
Risk Category
Risk Category is defined based on end of Probe 2 provider error rates. The categories are defined as:
| Risk Category | Error Rate |
|---|---|
|
Minor |
0–20% |
|
Major |
21–100% |
E/M 99232/99233 — Subsequent Hospital Care
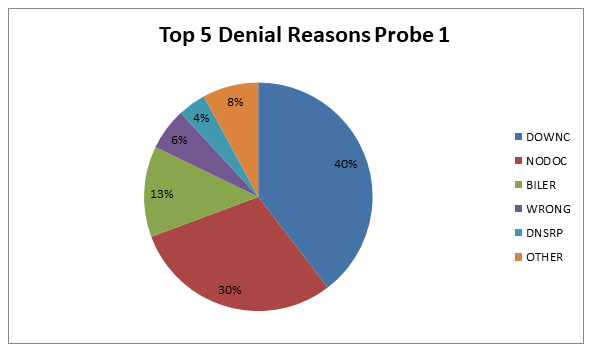
Top 5 Denial Reasons Probe 1 January 2, 2018, to February 28, 2020
- DOWNC — Payer deems the information submitted does not support this level of service; downcoded
- NODOC — Documentation requested for this date of service was not received or was incomplete
- BILER — Claim billed in error per provider
- WRONG — Documentation received contains an incorrect/incomplete/illegible patient identification or date of service
- DNSRP — Documentation not signed by the billing provider
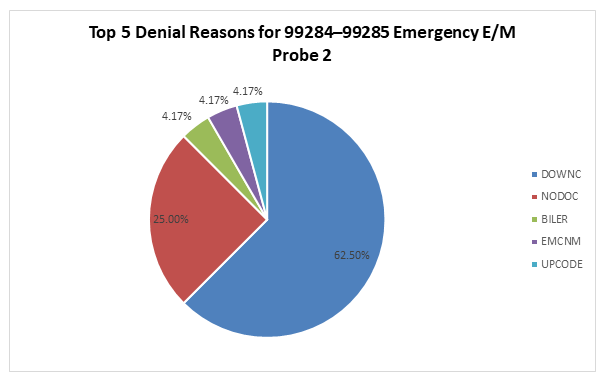
E/M 99232/99233 — Subsequent Hospital Care: Probe 2
Top 5 Denial Reasons January 2, 2018, to February 28, 2020
- DOWNC — Payer deems the information submitted does not support this level of service; downcoded
- NODOC — Documentation requested for this date of service was not received or was incomplete
- UPCODE — Payer deems the information submitted does not support this level of service; upcoded
- BILER — Claim billed in error per provider
DOWNC
Payer deems the information submitted does not support this level of service; downcoded.
- Ensure that all documentation to support the level of service billed is submitted for review
- Verify that documentation to support the level of service billed is included. Please refer to the website at www.PalmettoGBA.com/medicare for links to applicable LCDs, NCDs and the E/M Scoresheet Tool for documentation requirements.
NODOC
Documentation requested for this date of service was not received or was incomplete.
- Submit all documentation related to the services billed within 45 days of the date on the ADR letter
- Review documentation prior to submission to ensure that the documentation is complete and that all dates of service requested are included
- Include any additional information pertinent to the date of service requested to support the services billed. For example: original chart notes, diagnostic, radiological or laboratory results.
- For claims denied with a M127 or N29 code listed on the remittance advice, be sure to submit all documentation for all dates of service on that claim with a reopen/redetermination request form by fax to (803) 699–2427
BILER
Claim billed in error per provider.
- Prior to billing claims, review the information to determine that the correct information is listed in the appropriate fields
- For all claims previously billed and denied by medical review, do not re-submit the claims. If you disagree with the decision from Medical Review, you must submit the appropriate documentation with a completed redetermination request form to the Appeals Department. This information can be sent by fax to (803) 699–2427.
- If documentation indicates that both an NPP and a physician performed the service, and the claim is billed under the physician’s NPI, the billing physician must sign the record
- Additionally, the documentation must include a statement that the billing provider had face-to-face contact with the patient and performed a substantive portion of the E/M visit. (A substantive portion of the E/M visit includes at least one of the three key components: history, exam or medical decision-making.)
- If documentation occurs in a teaching environment, review the documentation to ensure that the billing provider has provided a teaching attestation and a signature
WRONG
Documentation received contains an incorrect/incomplete/illegible patient identification or date of service.
- Review all documentation prior to submission to ensure that it is for the correct patient and date of service
- Ensure that patient identifiers are legible and complete
- Ensure that the complete date of service is clearly and legibly noted on all documentation
- Prior to billing claims, review the information to determine that the correct patient identifier and the correct date of service are listed in the appropriate field
DNSRP
Documentation not signed by the rendering provider.
- Verify that all documentation is legibly signed by the correct rendering physician or nonphysician practitioner
- Verify that electronic signature meets the CMS signature requirements as listed in the article “Medicare Medical Records: Signature Requirements Acceptable and Unacceptable Practices” located on our website at www.PalmettoGBA.com
- Submit a valid Signature Attestation with any documentation that lacks the correct rending provider's signature. Do not resubmit altered documentation with late added provider signature. This will not be accepted by medical review. For an example of a signature attestation, refer to the article “Medicare Medical Records: Signature Requirements Acceptable and Unacceptable Practices” located on our website at www.PalmettoGBA.com.
UPCODE
Payer deems the information submitted does not support this level of service; upcoded.
- Ensure that all documentation to support the level of service billed is submitted for review
- Verify that documentation to support the level of service billed is included. Please refer to the website at www.PalmettoGBA.com for links to applicable LCDs, NCDs and the E/M Scoresheet Tool for documentation requirements.
Education
Providers are offered an individualized education session where each claim denial will be discussed, and any questions will be answered. Palmetto GBA offers a variety of methods for provider education such as webinar sessions, web-based presentations, or teleconferences. Other education methods may also be available.
Next Steps
Providers found to be non-compliant (major risk category/denial rate of 21-100%) at the completion of TPE Probe 1 will advance to Probe 2, and providers found to be non-compliant (major risk category/denial rate of 21-100%) at the completion of TPE Probe 2 will advance to Probe 3 of TPE at least 45 days from completion of the 1:1 post probe education call date. Palmetto GBA offers education at any time for providers. Providers do not have to be identified for TPE to request education.
References
- CMS Targeted Probe and Educate (TPE) web page
- Change Request 10249 (PDF, 241.88 KB)