Targeted Probe and Educate Progress Update: Hospice - NCLOS
The Centers for Medicare & Medicaid Services (CMS) Change Request 10249 (PDF, 241.88 KB) implemented the Targeted Probe & Educate (TPE) process, effective October 1, 2017. The following provides Probe 1 TPE results statistics from October 1, 2017 – January 31, 2020.
Findings
Medical Review initiated Probe review edits for providers identified through data analysis demonstrating high risk for improper payment. Providers have been offered education throughout and upon completion of the Probe 1 TPE review. Current Probe 1 Hospice Non-Cancerous Length of Stay (NCLOS) Results are as follows:
Non-Cancerous Length of Stay (NCLOS)
Probes Processed October 1, 2017 – January 31, 2020
| Number of Providers with Edit Effectiveness Performed | Providers Compliant Completed/Removed After Probe 1 | Providers Non-Compliant Progressing to TPE Probe 2 | Providers Removed for Other Reasons | Overall Charge Denial Rate |
|---|---|---|---|---|
|
110 |
87 |
20 |
3 |
15% |
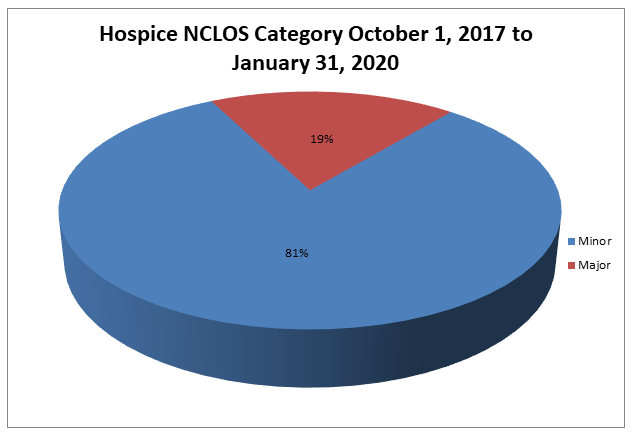
Risk Category
Risk Category is defined based on end of Probe 1 provider error rates. The categories are defined as:
| Risk Category | Error Rate |
|---|---|
|
Minor |
0–20% |
|
Major |
21–100% |
Hospice NCLOS
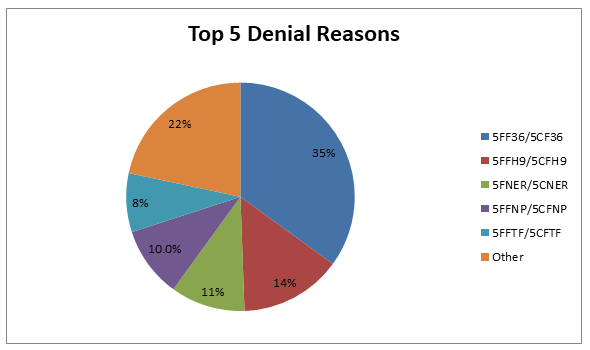
Top 5 Denial Reasons October 1, 2017 – January 31, 2020
- 5FF36/5CF36 — Documentation Submitted Does Not Support Prognosis of Six Months or Less
- 5FFH9/5CFH9 — Physician Narrative Statement Not Present or Not Valid
- 5FNER/5CNER — The Hospice Election Statement Does Not Meet Statutory/Regulatory Requirements
- 5FFNP/5CFNP — No Plan of Care
- 5FFTF/5CFTF — Face to Face Encounter Requirements Not Met
5FF36/5CF36 – Documentation Submitted Does Not Support Prognosis of Six Months or Less
Reason for Denial
The claim has been fully or partially denied because the documentation submitted for review did not support prognosis of six months or less.
How to Avoid a Denial
- Ensure a legible signature is present on all documentation necessary to support six-month prognosis
- Submit documentation for review to provide clear evidence the beneficiary has a six-month or fewer prognoses which supports hospice appropriateness at the time the benefit is elected, and continues to be hospice appropriate for the dates of service billed
- Palmetto GBA has a Local Coverage Determination (LCD) for some non-cancer diagnoses. Submit documentation which supports the coverage criteria outlined in the policy. If documenting weight loss to demonstrate a decline in condition, include how much weight was lost over what period of time, past and current nutritional status, current weight and any related interventions.
- Document any comorbidity which may further support the terminal condition of the beneficiary and the continuing appropriateness of hospice care
5FNER/5CNER — The Hospice Election Statement Does Not Meet Statutory/Regulatory Requirements
Reason for Denial
The Hospice Election Statement did not include the effective date of the election. Statutory/regulatory requirements were not met.
How to Avoid a Denial
A Medicare beneficiary must complete an election statement before the Hospice Medicare Benefit can begin. The election statement must include the following items of information:
- Identification of the particular hospice that will provide care to the individual
- The individual’s or representative’s (as applicable) acknowledgment that the individual has been given a full understanding of hospice care, particularly the palliative rather than curative nature of treatment
- The individual’s or representative’s (as applicable) acknowledgment that the individual understands that certain Medicare services are waived by the election
- The effective date of the election, which may be the first day of hospice care or a later date, but may be no earlier than the date of the election statement. An individual may not designate an effective date that is retroactive
- The individual’s designated attending physician (if any). Information identifying the attending physician recorded on the election statement should provide enough detail so that it is clear which physician or nurse practitioner (NP) was designated as the attending physician. This information should include, but is not limited to, the attending physician’s full name, office address, NPI number, or any other detailed information to clearly identify the attending physician.
- The individual’s acknowledgment that the designated attending physician was the individual’s or representative’s choice
- The signature of the individual or representative
5FFH9/5CFH9 — Physician Narrative Statement Not Present or Not Valid
Reason for Denial
The claim has been denied as the physician narrative statement is not present or not valid.
How to Avoid a Denial
- The physician must include a brief narrative explanation of the clinical findings that supports a life expectancy of 6 months or less as part of the certification and recertification forms, or as an addendum to the certification and recertification forms
- If the narrative is part of the certification or recertification form, then the narrative must be located immediately prior to the physician’s signature
- If the narrative exists as an addendum to the certification or recertification form, in addition to the physician’s signature on the certification or recertification form, the physician must also sign immediately following the narrative in the addendum
- The narrative shall include a statement under the physician signature attesting that by signing, the physician confirms that he/she composed the narrative based on his/her review of the patient’s medical record or, if applicable, his or her examination of the patient
- The narrative must reflect the patient’s individual circumstances and cannot contain check boxes or standard language used for all patients
5FFNP/5CFNP — No Plan of Care
Reason for Denial
The claim has been fully or partially denied as documentation submitted for review did not include a plan of care for all or some of the dates billed.
Claims with dates of service beginning July 19, 2010, require that a valid plan of care (POC) be included as part of the medical review process according to Change Request 6982.
How to Avoid a Denial
- The hospice must submit POCs for dates of service billed when responding to ADR request
- All dates billed must be covered by a plan of care to be payable under the Medicare hospice benefit
- If more than one plan of care covers the dates of service in question, submit all the related plans of care for review
- The POC must contain certain information to be considered valid. This includes
- Scope and frequency of services to meet the beneficiary’s/family’s needs
- Beneficiary specific information, such as assessment of the beneficiary's needs, management of discomfort and symptom relief
- Services that are reasonable and necessary for the palliation and management of the beneficiary’s terminal illness and related conditions
The plan of care must specify the hospice care and services necessary to meet the patient and family-specific needs identified in the comprehensive assessment.
All hospice care and services must follow an individualized written plan of care.
The plan of care must be reviewed, revised and documented as frequently as the beneficiary's condition requires, but no less frequently than every fifteen (15) calendar days.
5FFTF/5CFTF — Face to Face Encounter Requirements Not Met
Reason for Denial
The services billed were not covered because the documentation submitted for review did not include documentation of a face to face encounter.
How to Avoid a Denial
The face to face encounter must occur no more than 30 calendar days prior to the start of the third benefit period and no more than 30 calendar days prior to every subsequent benefit period thereafter.
Specific documentation related to face to face encounter requirements must be submitted for review. This includes, but is not limited to, the following:
- The hospice physician or nurse practitioner who performs the encounter must attest in writing that he or she had a face to face encounter with the patient, including the date of the encounter
- The attestation, its accompanying signature, and the date signed, must be separate and distinct section of, or an addendum to, the recertification form, must be clearly titled
• When a nurse practitioner performs the encounter, the attestation must state that the clinical findings of that visit were provided to the certifying physician for use in determining whether the patient continues to have a life expectancy of 6 months or less, should the illness run its normal course
• The face to face encounter requirement documentation
Education
Providers are offered an individualized education session where each claim denial will be discussed and any questions will be answered. Palmetto GBA offers a variety of methods for provider education such as webinar sessions, web-based presentations, or teleconferences. Other education methods may also be available.
Next Steps
Providers found to be non-compliant (major risk category/denial rate of 21–100%) at the completion of TPE Probe 1 will advance to Probe 2, and providers found to be non-compliant (major risk category/denial rate of 21–100%) at the completion of TPE Probe 2 will advance to Probe 3 of TPE at least 45 days from completion of the 1:1 post probe education call date. Palmetto GBA offers education at any time for providers. Providers do not have to be identified for TPE to request education.