Targeted Probe and Educate Progress Update for JM Home Health Bene Sharing
Published 03/12/2020
The Centers for Medicare & Medicaid Services (CMS) Change Request 10249 (PDF, 241.88 KB) implemented the Targeted Probe and Educate (TPE) process, effective October 1, 2017. The following provides Probe 1 and Probe 2 TPE results statistics from October 1, 2017, to January 31, 2020.
Findings
Medical Review initiated Probe review edits for providers identified through data analysis demonstrating high risk for improper payment. Providers have been offered education throughout and upon completion of the Probe 1 and Probe 2 TPE review. Current Probe 1 Home Health Bene Sharing TPE Results are as follows:
Medical Review initiated Probe review edits for providers identified through data analysis demonstrating high risk for improper payment. Providers have been offered education throughout and upon completion of the Probe 1 and Probe 2 TPE review. Current Probe 1 Home Health Bene Sharing TPE Results are as follows:
Home Health
Probes Processed October 1, 2017 – January 31, 2020
Probes Processed October 1, 2017 – January 31, 2020
|
Number of Providers with Edit Effectiveness Performed Probe 1
|
Providers Compliant Completed/ Removed After Probe 1
|
Providers Non-Compliant Progressing to TPE Probe 2
|
Providers Removed for Other Reason
|
Number of Providers with Edit Effectiveness Performed Probe 2
|
Providers Compliant Completed/ Removed After Probe 2 |
Providers Non-Compliant Progressing to TPE Probe 3 |
|---|---|---|---|---|---|---|
|
35
|
29
|
6
|
0
|
0
|
0 |
0 |
Findings by State
Palmetto GBA’s overview of results by state, for providers who have had edit effectiveness performed, for Probe 1 and Probe 2 TPE review from October 1, 2017 – January 31, 2020.
|
State
|
Number of Providers with Edit Effectiveness Performed Probe 1
|
Providers Compliant Completed / Removed After Probe 1
|
Providers Non-Compliant Progressing to TPE Probe 2
|
Providers Removed from Probe 1 or 2 for Other Reason
|
Number of Providers with Edit Effectiveness Performed Probe 2
|
Providers Compliant Completed/ Removed After Probe 2
|
Providers Non-Compliant Progressing to TPE Probe 3
|
|---|---|---|---|---|---|---|---|
|
Alabama
|
9
|
9
|
0
|
0
|
0
|
0
|
0 |
|
Arkansas
|
1
|
1
|
0
|
0
|
0
|
0
|
0 |
|
Florida
|
25
|
19
|
6
|
0
|
0
|
0
|
0 |
|
Georgia
|
0
|
0
|
0
|
0
|
0
|
0
|
0 |
|
Illinois |
0 |
0 |
0 |
0 |
0 |
0 |
0 |
|
Indiana
|
0
|
0
|
0
|
0
|
0
|
0
|
0 |
|
Kentucky
|
0
|
0
|
0
|
0
|
0
|
0
|
0 |
|
Louisiana
|
0
|
0
|
0
|
0
|
0
|
0
|
0 |
|
Mississippi
|
0
|
0
|
0
|
0
|
0
|
0
|
0 |
|
New Mexico
|
0
|
0
|
0
|
0
|
0
|
0
|
0 |
|
N. Carolina
|
0
|
0
|
0
|
0
|
0
|
0
|
0 |
|
Ohio
|
0
|
0
|
0
|
0
|
0
|
0
|
0 |
|
Oklahoma
|
0
|
0
|
0
|
0
|
0
|
0
|
0 |
|
Other
|
0
|
0
|
0
|
0
|
0
|
0
|
0 |
|
S. Carolina
|
0
|
0
|
0
|
0
|
0
|
0
|
0 |
|
Tennessee
|
0
|
0
|
0
|
0
|
0
|
0
|
0 |
|
Texas
|
0
|
0
|
0
|
0
|
0
|
0
|
0 |
|
ZPIC
|
0
|
0
|
0
|
0
|
0
|
0
|
0 |
| State | Overall Charge Denial Rate Per State Probe 1 | Overall Charge Denial Rate Per State Probe 2 |
|---|---|---|
|
Alabama |
4.53% |
N/A |
|
Arkansas |
4.00% |
N/A |
|
Florida |
13.46% |
N/A |
|
Georgia |
N/A |
N/A |
|
Illinois |
N/A |
N/A |
|
Indiana |
N/A |
N/A |
|
Kentucky |
N/A |
N/A |
|
Louisiana |
N/A |
N/A |
|
Mississippi |
N/A |
N/A |
|
North Carolina |
N/A |
N/A |
|
New Mexico |
N/A |
N/A |
|
Ohio |
N/A |
N/A |
|
Oklahoma |
N/A |
N/A |
|
Other |
N/A |
N/A |
|
South Carolina |
N/A |
N/A |
|
Tennessee |
N/A |
N/A |
|
Texas |
N/A |
N/A |
|
ZPIC |
N/A |
N/A |
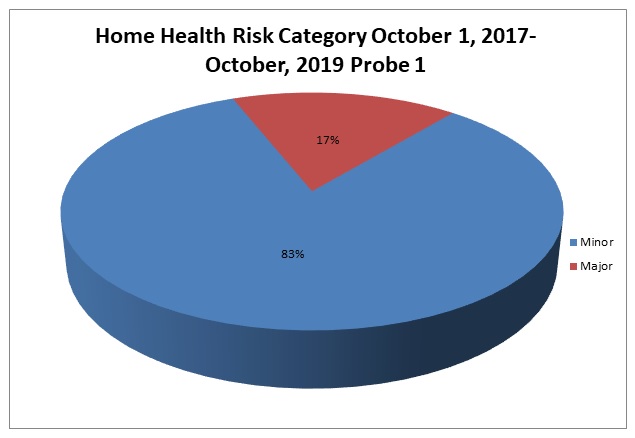
Risk Category
Risk Category is defined based on end of Probe 1 provider error rates. The categories are defined as:
Risk Category is defined based on end of Probe 1 provider error rates. The categories are defined as:
|
Risk Category
|
Error Rate
|
|---|---|
|
Minor
|
0–20 %
|
|
Major
|
21–100 %
|
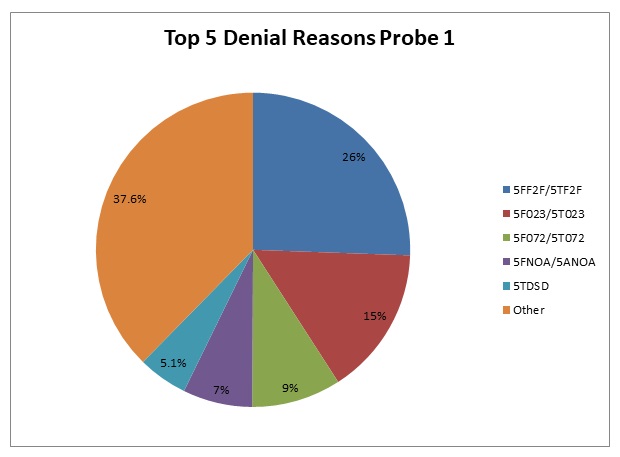
Home Health Probe 1 TPE
Top 5 Denial Reasons October 1, 2017 — January 31, 2020
-
5FF2F/5TF2F — Face-to-Face Encounter Requirements Not Met
-
5F023/5T023 — No Plan of Care or Certification
-
5F072/5T072 — No Physician’s Order for Services or More than Ordered
-
5FNOA/5ANOA — No Initial OASIS/OASIS Present for SCIC HIPPS Code
-
5TDSD — Dependent Services Denied (Qualifying Service Denied Technically)
5FF2F/5TF2F
Reason for Denial
The services billed were not covered because the documentation submitted for review did not include (adequate) documentation of a face-to-face encounter.
The services billed were not covered because the documentation submitted for review did not include (adequate) documentation of a face-to-face encounter.
How to Avoid a Denial
Specific documentation related to face to face encounter requirements must be submitted for review. This includes, but is not limited to, the following:
Specific documentation related to face to face encounter requirements must be submitted for review. This includes, but is not limited to, the following:
-
A face-to-face encounter must occur no more than 90 days prior to the home health start of care date or within 30 days of the start of the home health care;
-
Encounter was related to the primary reason the patient requires home health services; and
-
Encounter was performed by a physician or allowed nonphysician practitioner
The certifying physician must also document the date of the face-to-face encounter. The face-to-face encounter can be performed by:
-
The certifying physician;
-
The physician who cared for the patient in an acute or post-acute care facility (from which the patient was directly admitted to home health);
-
A nurse practitioner or a clinical nurse specialist who is working in collaboration with the certifying physician or the acute/post-acute care physician; or
-
A certified nurse midwife or physician assistant under the supervision of the certifying physician or the acute/post-acute care physician
The certifying physician’s and/or the acute/post-acute care facilities medical record for the patient must contain the actual clinical note for the face-to-face encounter visit that demonstrates that the encounter:
-
Occurred within the required timeframe;
-
Was related to the primary reason the patient requires home health services; and
-
Was performed by an allowed provider type
This information can be found most often in, but is not limited to the following examples:
-
Discharge Summary;
-
Progress Note;
-
Progress Note and Problem List; or
-
Discharge Summary and Comprehensive Assessment
5F023/5T023
Reason for Denial
The services billed were not covered because the home health agency (HHA) did not have the plan of care established and approved by a physician, as required by Medicare, included in the medical records submitted for review and/or the service(s) billed were not covered because the documentation submitted did not include the physician’s signed certification or recertification.
The services billed were not covered because the home health agency (HHA) did not have the plan of care established and approved by a physician, as required by Medicare, included in the medical records submitted for review and/or the service(s) billed were not covered because the documentation submitted did not include the physician’s signed certification or recertification.
How to Avoid a Denial
-
Ensure that the appropriate plan of care (POC) is included and that it is legibly signed and dated by the physician prior to billing
-
A plan of care refers to the medical treatment plan established by the treating physician with the assistance of the home health skilled professional. The plan of care contains all pertinent diagnoses, the patient’s mental status, the types of services, supplies, and equipment required, the frequency of visits to be made, prognosis, rehabilitation potential, functional limitations, activities permitted, nutritional requirements, all medications and treatments, safety measures to protect against injury, instructions for timely discharge or referral and any additional items the HHA or physician chooses to include.
-
Ensure that the signed certification or recertification is submitted when responding to an ADR
-
The physician must certify that:
-
The home health services were required because the individual was confined to his/her home and needs intermittent skilled nursing care, physical therapy and/or speech-language pathology, or continues to need occupational therapy;
-
A plan for furnishing such services to the individual has been established and is periodically reviewed by a physician; and
-
The services were furnished while the individual was under the care of a physician
-
-
Since the certification is closely associated with the plan of care, the same physician who establishes the plan must also certify to the necessity for home health services. Certifications must be obtained at the time the plan of care is established or as soon thereafter as possible. There is no requirement that a specific form must be used, as long as the intermediary can determine that this requirement is met. When requesting reimbursement for a claim, the provider must have the certification on file and be able to submit this information if medical records are requested by the intermediary.
-
The physician must recertify at intervals of at least once every 60 days that there is a continuing need for services and should estimate how long services will be needed. The recertification should be obtained at the time the plan of care is reviewed and must be signed by the same physician who signs the plan of care. When requesting reimbursement for a claim, the provider must have the recertification on file and be able to submit this information if medical records are requested by the intermediary.
5F072/5T072
Reason for Denial
Medicare requires that all services be ordered (including discipline, duration, frequency, treatment, legible, signed/dated appropriately) by a physician. The denied visits were not ordered, or exceeded the physician's orders.
Reason for Denial
Medicare requires that all services be ordered (including discipline, duration, frequency, treatment, legible, signed/dated appropriately) by a physician. The denied visits were not ordered, or exceeded the physician's orders.
How to Avoid a Denial
-
When responding to an Additional Development Request (ADR), verify orders for all services rendered and billed are included with the medical records
- Ensure physician orders for all services billed are obtained prior to providing the service and prior to billing the final payment claim to Medicare
5FNOA/5ANOA
Reason for Denial
Medical necessity was not supported as there is no Outcome and Assessment Information Set (OASIS) present in the state repository for the initial HIPPS code billed on the claim.
Medical necessity was not supported as there is no Outcome and Assessment Information Set (OASIS) present in the state repository for the initial HIPPS code billed on the claim.
How to Avoid a Denial
To avoid denials for this reason, the provider should ensure that the OASIS that generated the HIPPS codes on the claim is submitted with the medical records in response to an Additional Development Request (ADR).
To avoid denials for this reason, the provider should ensure that the OASIS that generated the HIPPS codes on the claim is submitted with the medical records in response to an Additional Development Request (ADR).
Under the Prospective Payment System (PPS), an OASIS is a regulatory requirement. The OASIS that generated the initial HIPPS code is necessary to determine the medical necessity of the level of care billed. Appropriate payment for the entire episode cannot be determined without the OASIS for the initial HIPPS code. As a result, all of the services billed are non-covered.
5TDSD
Reason for Denial
In order to allow dependent services, a qualifying skilled service such as nursing, physical therapy, speech language pathology and/or continuing occupational therapy must be ordered and medically necessary. Since the qualifying skilled service was denied/non-covered, the supportive services were also denied/non-covered.
In order to allow dependent services, a qualifying skilled service such as nursing, physical therapy, speech language pathology and/or continuing occupational therapy must be ordered and medically necessary. Since the qualifying skilled service was denied/non-covered, the supportive services were also denied/non-covered.
How to Avoid a Denial
Ensure that the qualifying skilled service documentation submitted meets all technical requirements and supports the medical necessity of the services billed when responding to an Additional Development Request (ADR).
Ensure that the qualifying skilled service documentation submitted meets all technical requirements and supports the medical necessity of the services billed when responding to an Additional Development Request (ADR).
Education
Providers are offered an individualized education session where each claim denial will be discussed, and any questions will be answered. Palmetto GBA offers a variety of methods for provider education such as webinar sessions, web-based presentations, or teleconferences. Other education methods may also be available.
Providers are offered an individualized education session where each claim denial will be discussed, and any questions will be answered. Palmetto GBA offers a variety of methods for provider education such as webinar sessions, web-based presentations, or teleconferences. Other education methods may also be available.
Next Steps
Providers found to be non-compliant (major risk category/denial rate of 21–100%) at the completion of TPE Probe 1 will advance to Probe 2, and providers found to be non-compliant (major risk category/denial rate of 21–100%) at the completion of TPE Probe 2 will advance to Probe 3 of TPE at least 45 days from completion of the 1:1 post probe education call date. Palmetto GBA offers education at any time for providers. Providers do not have to be identified for TPE to request education.
Providers found to be non-compliant (major risk category/denial rate of 21–100%) at the completion of TPE Probe 1 will advance to Probe 2, and providers found to be non-compliant (major risk category/denial rate of 21–100%) at the completion of TPE Probe 2 will advance to Probe 3 of TPE at least 45 days from completion of the 1:1 post probe education call date. Palmetto GBA offers education at any time for providers. Providers do not have to be identified for TPE to request education.