Targeted Probe and Educate Progress Update: Hospice - GIP - General Inpatient Care
The Centers for Medicare & Medicaid Services (CMS) Change Request 10249 (PDF, 241.88 KB) implemented the Targeted Probe and Educate (TPE) process, effective October 1, 2017. The following provides Probe 1 TPE results statistics from October 1, 2017, to January 31, 2020.
Findings
Medical Review initiated Probe review edits for providers identified through data analysis demonstrating high risk for improper payment. Providers have been offered education throughout and upon completion of the Probe 1 TPE review. Current Probe 1 Hospice - GIP - General Inpatient Care Results are as follows:
GIP — General Inpatient Care
Probes Processed October 1, 2017 – January 31, 2020
| Number of Providers with Edit Effectiveness Performed | Providers Compliant Completed/Removed After Probe 1 | Providers Non-Compliant Progressing to TPE Probe 2 | Providers Removed for Other Reasons | Overall Charge Denial Rate |
|---|---|---|---|---|
|
30 |
29 |
1 |
0 |
4% |
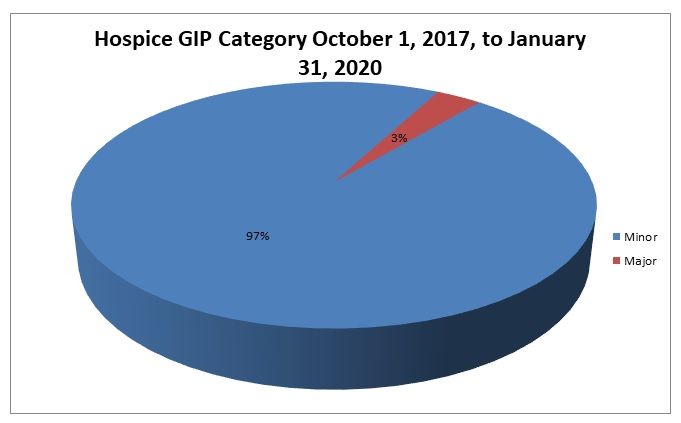
Risk Category
Risk Category is defined based on end of Probe 1 provider error rates. The categories are defined as:
|
Risk Category
|
Error Rate
|
|---|---|
|
Minor
|
0–20 %
|
|
Major
|
21–100 %
|
Hospice GIP — General Inpatient Care
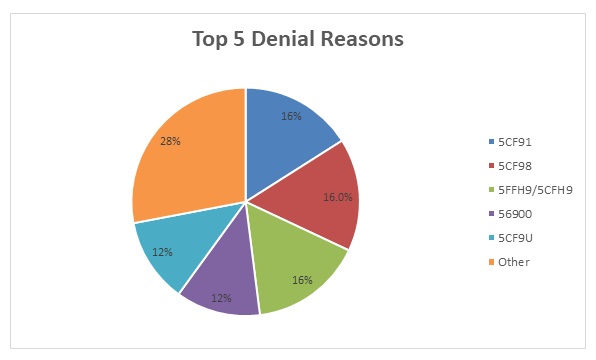
Top Denial Reasons October 1, 2017 – January 31, 2020
- 5CF91 — Hospice General Inpatient Reduction — Services Not Reasonable and Necessary
- 5CF98 — The day of discharge from an Inpatient Facility is paid at the Routine Home Care rate. The Hospice Inpatient Level of Care is reduced to the Hospice Routine Care Rate for this date.
- 5FFH9/5CFH9 — Physician Narrative Statement Not Present or Not Valid
- 56900 — Auto Deny — Requested Records Not Submitted Timely
- 5CF9U — Hospice GIP Reduction — Services Not Due to Terminal Illness
5CF91 — Hospice General Inpatient Reduction — Services Not Reasonable and Necessary
Reason for Denial
The hospice services billed for general inpatient care days were not covered, as submitted documentation did not support medical necessity. Therefore, the general inpatient care days were reduced to routine care days.
How to Avoid a Denial
The hospice benefit allows for general inpatient care services if the hospital stay is reasonable and necessary. Documentation should include the following:
- Name of the contract facility in which the patient is receiving general inpatient care
- Explanation for admission to the inpatient facility
- Hospice interdisciplinary notes during the general inpatient stay and the physician’s discharge summary
- Documentation of the patient’s condition during the inpatient stay
Hospitalization must be on a short-term basis and must be related to complications attributable to the terminal diagnosis such as pain control or symptom management which cannot be provided in other settings.
In order to avoid denials for this reason, the documentation submitted must include the following:
- Need for pain control or symptom management that is not feasible in other settings
- Skilled care required when home support has broken down and it is no longer feasible to furnish needed care in the home setting
- Patient’s need for medication adjustment, observation or other stabilizing treatments, which cannot be furnished in home
For further information on the above Medicare coverage issue, references include, but are not limited to the following:
- CMS Manual System, Pub 100-02, Medicare Benefit Policy Manual, Chapter 9, Section 40.1.5
- CMS Manual System, Pub 100-04, Medicare Claims Processing Manual, Chapter 11, Section 30.1
5CF98 — The day of discharge from an Inpatient Facility is paid at the Routine Home Care rate. The Hospice Inpatient Level of Care is reduced to the Hospice Routine Care Rate for this date.
Reason for Denial
The day of discharge from the Inpatient Level of Care is paid at the Routine Home Care rate.
How to Avoid a Denial
Any day of which the beneficiary is in an inpatient approved facility for inpatient care, the appropriate inpatient rate (general or respite) is paid depending on the category of care furnished. The inpatient rate (general or respite) is paid for the date of admission and all subsequent inpatient days, except the day on which the patient is discharged. For the day of discharge, the appropriate home care rate is paid unless the patient dies as an inpatient.
5FFH9/5CFH9 — Physician Narrative Statement Not Present or Not Valid
Reason for Denial
The claim has been denied as the physician narrative statement is not present or not valid.
How to Avoid a Denial
- The physician must include a brief narrative explanation of the clinical findings that supports a life expectancy of six months or less as part of the certification and recertification forms, or as an addendum to the certification and recertification forms
- If the narrative is part of the certification or recertification form, then the narrative must be located immediately prior to the physician’s signature
- If the narrative exists as an addendum to the certification or recertification form, in addition to the physician’s signature on the certification or recertification form, the physician must also sign immediately following the narrative in the addendum
- The narrative shall include a statement under the physician signature attesting that by signing, the physician confirms that he/she composed the narrative based on his/her review of the patient’s medical record or, if applicable his or her examination of the patient
- The narrative must reflect the patient’s individual circumstances and cannot contain check boxes or standard language used for all patients
56900 — Auto Deny — Requested Records Not Submitted Timely
Reason for Denial
Requested medical records were not received within the 45-day time limit. Therefore, we are unable to determine the medical necessity of the service billed and this claim has been denied. If less than 120 days after denial notification on the remittance advice, submit records to the contractor requesting records at the address listed on the original Additional Development Request (ADR) to request reopening. Do not resubmit the claim.
How to Avoid a Denial
- Be aware of the Additional Development Request (ADR) date and the need to submit medical records within 45 days of the ADR date
- Submit the medical records as soon as the Additional Development Request (ADR) is received
- Monitor the status of your claims in Direct Data Entry (DDE) and begin gathering the medical records as soon as the claim goes to the location of SB6001
- Return the medical records to the address on the Additional Development Request (ADR). Be sure to include the appropriate mail code or station number. This ensures that your responses are promptly routed to the Medical Review Department. Fax and electronic data submissions are also accepted as indicated on the Additional Development Request (ADR).
- Gather all of the information needed for the claim and submit it all at one time
- Attach a copy of the Additional Development Request (ADR) request to each individual claim
- If responding to multiple Additional Development Requests (ADRs), separate each response and attach a copy of the ADR to each individual set of medical records. Make sure each set of medical records is individually identifiable and bound securely to ensure that no documentation is detached or lost. Do not use paper clips.
- Do not mail packages C.O.D.; we cannot accept them
For more information, refer to the Palmetto GBA Web site at www.PalmettoGBA.com and then search for the following article: Medical Review Progressive Corrective Action (PCA) Process
5CF9U — Hospice GIP Reduction — Services Not Due to Terminal Illness
Reason for Denial
The hospice services for general inpatient care days were reduced to routine care days because the documentation submitted did not support the inpatient stay as being related to the terminal condition.
How to Avoid a Denial
The hospice benefit allows for general inpatient care services if the hospital stay is related to the patient’s terminal diagnosis. Documentation should include the following:
- The name of the contract facility in which the patient is receiving general inpatient care
- An explanation for admission to the inpatient facility
- Hospice interdisciplinary notes during the general inpatient stay
- The physician’s discharge summary
- Documentation of the patient’s condition during the inpatient stay
Hospitalization must be on a short-term basis and should relate to complications attributable to the terminal diagnosis such as pain control or symptom management, which cannot be provided in other settings.
For further information on the above Medicare coverage issue, references include, but are not limited to, these resources:
- CMS Manual System, Pub 100-02, Medicare Benefit Policy Manual, Chapter 9, Section 40.1.5
- CMS Manual System, Pub 100-04, Medicare Claims Processing Manual, Chapter 11, Section 30.1
Education
Providers are offered an individualized education session where each claim denial will be discussed, and any questions will be answered. Palmetto GBA offers a variety of methods for provider education such as webinar sessions, web-based presentations, or teleconferences. Other education methods may also be available.
Next Steps
Providers found to be non-compliant (major risk category/denial rate of 21–100%) at the completion of TPE Probe 1 will advance to Probe 2, and Providers found to be non-compliant (major risk category/denial rate of 21–100%) at the completion of TPE Probe 2 will advance to Probe 3 of TPE at least 45 days from completion of the 1:1 post probe education call date. Palmetto GBA offers education at any time for providers. Providers do not have to be identified for TPE to request education.
References
- CMS Targeted Probe and Educate (TPE) Web Page
- Change Request 10249 (PDF, 241.88 KB)