Requesting Prior Authorization for Repetitive, Scheduled Non-Emergent Ambulance Transports
On July 18, 2022, the RRB SMAC implemented the Repetitive, Scheduled Non-Emergent Ambulance Transport (RSNAT) Prior Authorization (PA) model for Railroad Medicare beneficiaries nationwide for transports on and after August 1, 2022.
Repetitive ambulance services are defined as medically necessary ambulance transport furnished in three or more round trips during a 10-day period, or at least one round trip per week for at least three weeks.
This PA model applies to independent ambulance suppliers that are not institutionally based providing Part B Medicare covered ambulance services billed on a CMS-1500 form and/or a HIPAA compliant ANSI X12N 837P electronic transaction.
Ambulance suppliers can submit a request for prior authorization of up to 40 non-emergency scheduled round trips (which equates to 80 one-way trips) in a 60-day period per prior authorization request. PA requests can be submitted for transports scheduled on and after August 1, 2022.
Prior authorization for RSNAT is voluntary but encouraged. If an ambulance supplier elects not to submit a prior authorization request before the fourth round-trip in a 30-day period, the RSNAT claim, and subsequent RSNAT claims, will be subject to a prepayment medical review.
Ambulance HCPCS Codes
The following ambulance HCPCS codes are subject to prior authorization under the model:
- A0426 — Ambulance service, Advanced Life Support (ALS), non-emergency transport, Level 1
- A0428 — Ambulance service, Basic Life Support (BLS), non-emergency transport
Associated service HCPCS code A0425 (ground mileage, per statute mile) should be billed with the appropriate transport code but is not subject to prior authorization.
We will not review prior authorization requests received for any code other than HCPCS code A0426 or A0428.
Number of Trips
A provisional affirmative prior authorization decision affirms a specified number of trips within a specific amount of time.
- The prior authorization decision, justified by the beneficiary’s condition, may affirm up to 40 round trips (which equates to 80 trips) per prior authorization request in a 60-day period
- An affirmative prior authorization decision may affirm less than 40 round trips, or affirm a request that seeks to provide a specified number of transports (40 round trips or less) in less than a 60-day period
- An affirmative decision can be for all or part of the requested number of trips
Transports exceeding 40 round trips (or 80 one-way trips) in a 60-day period will require an additional prior authorization request.
Extended Affirmation Periods for Beneficiaries with a Chronic Medical Condition
CMS allows Medicare Administrative Contractors (MACs), including the RRB Specialty MAC, to consider an extended affirmation period for beneficiaries with a chronic medical condition deemed not likely to improve over time. For an extended affirmation period to be allowed, the medical records must clearly indicate that the medical condition is chronic, and the MAC must have established through two previous prior authorization requests that the beneficiary’s medical condition has not changed or has deteriorated from previous requests before allowing an extended affirmation period.
The decision to allow an extended affirmation period is at MAC discretion. The maximum number of requested trips remains at 40 round trips (80 one-way trips).
Medicare’s prior authorization decision for requests meeting the above criteria may affirm up to 120 round trips (which equates to 240 one-way trips) per prior authorization request in a 180-day period.
Ambulance suppliers are still responsible for maintaining a valid Physician Certification Statement (PCS) at all times. The MAC reserve the right to request the PCS at any time.
Each individual patient transport must still be reasonable and necessary, regardless of whether a new prior authorization is required.
Submitting a Request
Methods of Submission
Submit your prior authorization request package to Railroad Medicare by one of the following methods:
- Palmetto GBA eServices portal — this is the method we encourage
- Fax to (803) 462–2632
- U.S. Mail to:
Palmetto GBA RRB RSNAT
PO Box 17089
Augusta, GA 30903-0001
- Electronic submission of medical documentation (esMD)
- For more information about esMD, see www.cms.gov/esMD
- For more information about esMD, see www.cms.gov/esMD
What to Include With Your Request
If you are submitting a PA request via fax, mail or esMD, please complete a Railroad Medicare Prior Authorization Request for Repetitive, Scheduled Non-Emergent Ambulance Transports Medicare Part B fax/mail Coversheet (PDF). Completing this form will help ensure we have all the information needed to complete your request.
Complete the following fields on the Prior Authorization Request form:
First, indicate your Request Type. Pick one of the following options:
- Initial
- An initial request is the first PA request for the 60-day PA period for the beneficiary, or a request for additional trips in the same 60-day period after the initial affirmation
- Resubmission
- A resubmission is any subsequent submissions to correct an error or omission identified after the initial prior authorization request decision was non-affirmed and prior to claim submission
- Choose when you are submitting corrections and/or additional information for a non-affirmed request with same PA request time period
- Enter the UTN of the most recent non-affirmed decision for the PA period
- Expedited
- Must explain why the standard timeframe for making a PA decision could jeopardize the life or health of the beneficiary.
- CMS expects requests for expedited reviews to be extremely rare as this model is for non-emergent services.
- Effective January 9, 2025, Palmetto GBA will not accept expedited PA review reques
Then complete the following fields:
- Number of transports requested
- Up to 80 one-way trips (equivalent of 40 round trips) can be requested for a 60-day period
- Enter the total number of trips, not round trips, requested
- Requested start date of the 60-day prior authorization period
- Cannot be before August 1, 2022, for Railroad Medicare
- HCPCS code and modifier(s)
- HCPCS code A0426 or A0428 only
- Modifier 1 — Enter both the origin and destination for round trip (example: HCPCS Modifiers RJ JR)
- Modifier 2 — Use if patient has a different origin or destination modifier for a separate type of transport
- Beneficiary information
- Beneficiary name
- Beneficiary Medicare Beneficiary Identifier (MBI)
- Beneficiary date of birth
- Do not submit more than one beneficiary on the Prior Authorization Request form
- Certifying physician information
- Certifying physician name
- Must match physician’s name on Physician Certification Statement (PCS)
- Certifying physician National Provider Identifier (NPI)
- Certifying physician Provider Transaction Access Number (PTAN) (optional)
- Certifying physician address
- Certifying physician name
- Ambulance supplier information
- Ambulance supplier name
- Ambulance supplier NPI
- Ambulance supplier PTAN
- Ambulance supplier address
- State in which ambulance is garaged
- Requestor/contact information
- Fax number (if a decision letter by fax is requested)
- Contact name and phone/extension (if different from requestor)
- Requestor name
- Requestor phone/extension
- Requestor signature
- Date of request
Documentation
In addition to the Prior Authorization Request form, your PA request package must contain the following:
- Information on the origin and destination of the transports
- Physician Certification Statement (PCS)
- The regulations governing PCS requirements for repetitive, scheduled, non-emergency ambulance services are specified at 42 CFR §410.40(e)(1) and (2)
- Must be dated and contain the signature and credentials of the certifying physician
- Documentation from the medical record to support the medical necessity of the transports
- Any other relevant document as deemed necessary by the MAC to process the prior authorization
The RSNAT PA model does not create new clinical documentation requirements or change existing Medicare ambulance coverage policies.
We encourage you to use the Ambulance Prior Authorization Documentation Decision Tool to help you determine whether the documentation you have to submit to request prior authorization of RSNAT is sufficient.
Submitting a PA Request Package through the eServices Portal
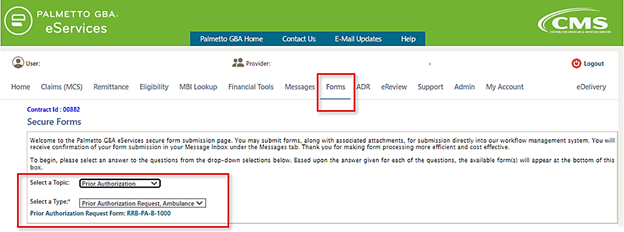
The secure online Prior Authorization Request-Ambulance form in the eServices portal will require the same information as the paper form. The Provider Information section will be pre-filled with the information related to the PTAN/NPI combination associated with the eServices user ID that you are logged in under, or the PTAN/NPI combination selected if you have multiple accounts linked to your user ID. You may then complete the Ambulance Prior Authorization Data section and upload attachments.
Once you complete all the required fields, you can attach your supporting documentation by uploading PDF files. The Ambulance Prior Authorization Documentation Decision Tool is built into the eServices PA Request form as a dynamic decision tree that will help you determine if your documentation is sufficient before you upload it.
Submitting your PA Request through eServices will allow you to track the submission of the form in your eServices Messages inbox as it goes through the PA review cycle. The eServices Messages inbox is searchable by document control number, patient, start date, etc. so you can easily locate your requests.
After You Submit a PA Request
Review Timeframes
Update: Effective January 9, 2025, Change Request (CR) 13711 (PDF) instructs the A/B Medicare Administrative Contractors (MACs) and the Railroad Retirement Board Specialty Medicare Administrative Contractor (RRB SMAC) to remove the option to request an expedited PA review, and to change the PA review timeframe from 10 business days to seven (7) calendar days under the RSNAT PA Model.
Initial and Resubmitted Requests
- For requests received before January 9, 2025, upon receipt of all relevant documentation, Palmetto GBA Railroad Medicare will review requests and postmark decision letters within 10 business days
- Effective January 9, 2025, upon receipt of all relevant documentation, we will review requests and postmark decision letters within seven (7) calendar days of receipt
Expedited Circumstances
- For requests received prior to January 9, 2025, Palmetto GBA Railroad Medicare will make reasonable efforts to communicate a decision within two business days of receipt of all applicable Medicare-required documentation
- Effective January 9, 2025, we will not accept expedited PA review requests
Review Decisions
A PA request can either be:
- Provisionally affirmed: A provisional affirmative decision is a preliminary finding that a future claim submitted to Medicare for the service likely meets Medicare’s coverage, coding, and payment requirements
- Non-affirmed: A non-affirmative decision is a preliminary finding that a future claim submitted to Medicare for the service does not meet Medicare’s coverage, coding, and payment requirements.
Note, the review decision is not a claim payment decision.
Unique Tracking Number (UTN)
Each completed prior authorization request is assigned a 14-byte unique tracking number (UTN). This number is included on the decision letter and will be used when submitting claims. A non-affirmed UTN will also be used when you send a resubmission for a non-affirmed PA request.
Letters
Railroad Medicare will send letters at the completion of the review to communicate the prior authorization request decision.
- If we are unable to make an affirmed or non-affirmed decision due to missing information on the PA Request form, we will send an Incomplete Request Letter to the provider. The letter will contain the reason the request was determined to be incomplete.
- If the decision is provisionally affirmed, we will send a decision letter with an affirmative Unique Tracking Number (UTN) to the provider and the beneficiary. The letter will specify the number of transports allowed and the affirmed PA period.
- It the decision is non-affirmed, we will send a decision letter with a non-affirmative UTN to the provider and the beneficiary. We will also send a detailed letter to the provider to further explain the reason for the non-affirmative decision.
After an Affirmed Decision
After receiving an affirmative decision, the ambulance supplier should:
- Render the service to beneficiary
- Submit the claim with the UTN. Do not include the UTN on the claim line for the mileage code.
- Maintain all documentation and the affirmative UTN number
After a Non-Affirmed Decision
After receiving an affirmative decision, review the decision letter and determine your next step. You can either:
- Resubmit another complete package with the additional documentation showing Medicare requirements have been met, as noted in the prior detailed decision letter(s)
- Resubmissions are unlimited during the prior authorization process
- Non-affirmative decisions are not appealable during the PA process
Or,
- Render the service and submit the claim with the non-affirmative unique tracking number (UTN)
- Medicare will deny the claim
- All appeal rights are then available
- If applicable, file with beneficiary’s secondary insurance
Resubmitting a Prior Authorization Request
- Make the needed changes/additions to the prior authorization package and resubmit the package with a new PA Request form
- Railroad Medicare will review the PA request package and make a decision within 10 business days of the request. Decision letters will be sent as described in the Letters section above.
- Resubmissions for non-affirmed prior authorization requests are unlimited
Submitting a Claim with a UTN
The following instructions apply to RSNAT claims submitted after either an affirmed or a non-affirmed decision. The claim must be submitted with the 14-byte unique tracking number (UTN) from the decision letter.
- CMS-1500 claim form
- Submit the UTN in the first 14 positions in item 23
- All other data submitted in item 23 must begin in position 15
- Electronic claims
- Submit the UTN in either the 2300 — Claim Information loop or 2400 — Service Line loop in the Prior Authorization reference (REF) segment where REF01 = “G1” qualifier and REF02 = UTN
- Bill the mileage code on the same claim as the transport code but do not submit the UTN on the claim line for the mileage code
Appeals
The RSNAT PA model does not include a separate appeal process for a non-affirmative prior authorization request decisions. However, a non-affirmative prior authorization request decision does not prevent the supplier from submitting a claim. Submission of a non-affirmed claim and the resulting denial by Railroad Medicare would constitute an initial determination that would make the appeals process available for disputes by Railroad Medicare beneficiaries and suppliers.
References
- CMS Repetitive, Scheduled Non-Emergent Ambulance Transport Prior Authorization Model Operational Guide (PDF)
- Medicare Benefit Policy Manual, Chapter 10 (PDF)
- Medicare Claims Processing Manual, Chapter 15 (PDF)