Targeted Probe and Educate Progress Update: Infliximab J1745
The Centers for Medicare & Medicaid Services (CMS) Change Request 10249 (PDF, 241.88 KB) implemented the Targeted Probe & Educate (TPE) process, effective October 1, 2017. The following provides Probe 1 and Probe 2 TPE results statistics from October 1, 2017, January 31, 2020.
Findings
Medical Review initiated Probe review edits for providers identified through data analysis demonstrating high risk for improper payment. Providers have been offered education throughout and upon completion of the Probe 1 and Probe 2 TPE review. Current Probe 1 and Probe 2 Infliximab J1745 TPE Results are as follows:
Infliximab J1745
Probes Processed October 1, 2017 – January 31, 2020
| Number of Providers with Edit Effectiveness Performed Probe 1 | Providers Compliant Completed/Removed After Probe 1 | Providers Non-Compliant Progressing to TPE Probe 2 | Number of Providers with Edit Effectiveness Performed Probe 2 | Providers Compliant Completed/Removed After Probe 2 | Providers Non-Compliant Progressing to TPE Probe 3 | Providers Removed from Probe 1 or 2 for Other Reasons |
|---|---|---|---|---|---|---|
|
25 |
23 |
2 |
1 |
1 |
0 |
0 |
Findings by State
Palmetto GBA’s overview of results by state, for providers who have had edit effectiveness performed, for Probe 1 and Probe 2 TPE review from October 1, 2017, to January 31, 2020.
| State | Number of Providers with Edit Effectiveness Performed Probe 1 | Providers Compliant Completed/Removed After Probe 1 | Providers Non-Compliant Progressing to TPE Probe 2 | Providers Removed from Probe 1 or 2 for Other Reasons | Number of Providers with Edit Effectiveness Performed Probe 2 | Providers Compliant Completed/Removed After Probe 2 | Providers Non-Compliant Progressing to TPE Probe 3 |
|---|---|---|---|---|---|---|---|
| North Carolina |
9 |
9 |
0 |
0 |
0 |
0 |
0 |
| South Carolina |
2 |
2 |
0 |
0 |
0 |
0 |
0 |
| Virginia |
9 |
9 |
0 |
0 |
0 |
0 |
0 |
| West Virginia |
5 |
3 |
2 |
0 |
1 |
1 |
0 |
| State | Overall Charge Denial Rate Per State Probe 1 | Overall Charge Denial Rate Per State Probe 2 |
|---|---|---|
| North Carolina |
4.40% |
N/A |
| South Carolina |
1.43% |
N/A |
| Virginia |
4.69% |
N/A |
| West Virginia |
27.56% |
5.82% |
Risk Category
Risk Category is defined based on end of Probe 1 provider error rates. The categories are defined as:
| Risk Category | Error Rate |
|---|---|
|
Minor |
0–20% |
|
Major |
21–100% |
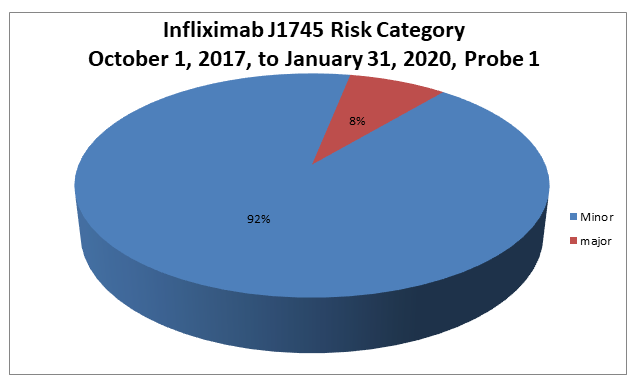
Risk Category
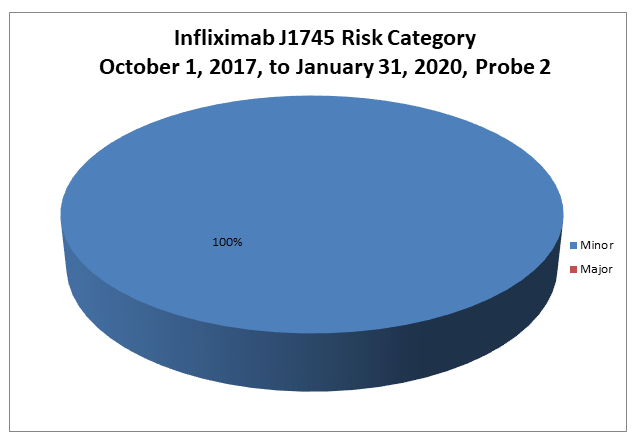
Risk Category is defined based on end of Probe 2 provider error rates. The categories are defined as:
| Risk Category | Error Rate |
|---|---|
|
Minor |
0–20% |
|
Major |
21–100% |
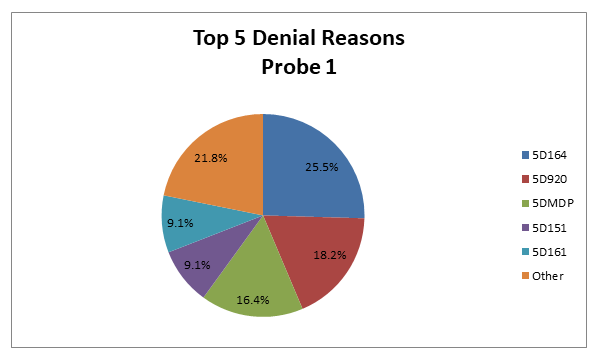
Infliximab J1745 Probe 1
Top 5 Denial Reasons October 1, 2017, to January 31, 2020
- 5D164 — No Documentation of Medical Necessity
- 5D920 — The Recommended Protocol Was Not Ordered and/or Followed
- 5DMDP — Dependent Services Denied (Qualifying Service Denied Medically)
- 5D151 — Units Billed More Than Ordered
- 5D161 — No Physician’s Orders
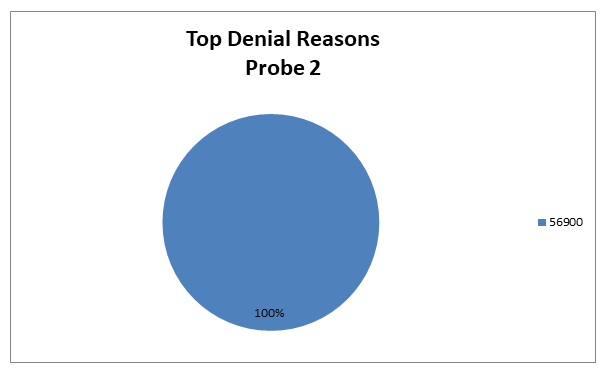
Infliximab J1745 Probe 2
Top Denial Reasons October 1, 2017, to January 31, 2020
- 56900 — Auto Deny — Requested Records Not Submitted Timely
5D164/5H164 — No Documentation of Medical Necessity
Reason for Denial
This claim was fully or partially denied because the documentation submitted for review does not support the medical necessity of some of the services billed.
How to Avoid a Denial
- Submit all documentation related to the services billed which support the medical necessity of the services.
- A legible signature is required on all documentation necessary to support orders and medical necessity.
- Use the most appropriate ICD-10-CM codes to identify the beneficiary’s medical diagnosis.
5D920/5H920 — The Recommended Protocol Was Not Ordered and/or Followed
Reason for Denial
Medicare cannot pay for this service because one or more requirements for coverage were not met.
How to Avoid a Denial
Documentation that may be helpful to avoid future denials for this reason may include, but are not limited to, the following:
- Clear physician’s order with indication of need, dose, frequency and route
- Date and time of associated chemotherapy, as applicable
- Relevant history and physical and/or progress notes
- Clear indication of the diagnosis
- Clinical signs and symptoms
- Prior treatment and response as applicable
- Stage of treatment as applicable
- Documentation of administration
5DMDP/5HMDP – Dependent Services Denied (Qualifying Service Denied Medically)
Reason for Denial
The dependent services will not be covered if the qualifying surgery has been denied. For example, the surgical procedure was denied as documentation did not support medical necessity, therefore all other charges cannot be allowed and will be denied as dependent to the medical denial of the qualifying service.
How to Avoid a Denial
Documentation that may be helpful to avoid future denials for this reason may include, but is not limited to, the following:
- All documentation to support orders, documentation of services rendered and documentation of medical necessity for the qualifying services for the date(s) billed
5D151/5H151 — Units Billed More Than Ordered
Reason for Denial
The physician’s orders submitted did not cover all of the units billed.
How to Avoid a Denial
In order to avoid unnecessary denials for this reason, the provider should ensure that the physician’s orders cover all the services to be billed prior to billing Medicare. When responding to an Additional Documentation Request (ADR), ensure that all orders for services billed are included with the medical records.
5D161/5H161 — No Physician’s Orders
Reason for Denial
This claim was fully or partially denied because there were no physician’s orders submitted for review for all or some of the services billed.
How to Avoid a Denial
- A physician’s order should be submitted for review with the request for copies of medical records
- A legible signature is required on all documentation necessary to support orders and medical necessity
- The copy of the order should be legible and dated
- Make sure any orders submitted for review are for the dates of service billed
56900 — Auto Deny — Requested Records Not Submitted Timely
Reason for Denial
The services billed were not covered because the claim was not submitted or not submitted timely in response to an Additional Documentation Request (ADR). When an ADR is generated, the provider has 45 days from the date the ADR was generated to respond with medical records. In accordance with CMS instructions, if the documentation needed to make a medical review determination is not received within 45 days from the date of the documentation request, Palmetto GBA will make a medical review determination based on the available medical documentation. If the claim is denied, payment will be denied, or an overpayment will be collected.
How to Avoid a Denial
- Be aware of the ADR date and the need to submit medical records within 45 days of the ADR date
- Submit the medical records as soon as the ADR is received
- Monitor the status of your claims in Direct Data Entry (DDE) and begin gathering the medical records as soon as the claim goes to the location of SB6001
- Return the medical records to the address on the ADR. Be sure to include the appropriate mail code or station number. This ensures that your responses are promptly routed to the Medical Review Department.
- Gather all of the information needed for the claim and submit it all at one time
- Attach a copy of the ADR request to each individual claim
- If responding to multiple ADR’s, separate each response and attach a copy of the ADR to each individual set of medical records. Make sure each set of medical records is bound securely with one staple in the upper left corner or a rubber band to ensure that no documentation is detached or lost. Do not use paper clips.
- Do not mail packages C.O.D.; we cannot accept them
Education
Providers are offered an individualized education session where each claim denial will be discussed, and any questions will be answered. Palmetto GBA offers a variety of methods for provider education such as webinar sessions, web-based presentations, or teleconferences. Other education methods may also be available.
Next Steps
Providers found to be non-compliant (major risk category/denial rate of 21–100%) at the completion of TPE Probe 1 will advance to Probe 2, and providers found to be non-compliant (major risk category/denial rate of 21–100%) at the completion of TPE Probe 2 will advance to Probe 3 of TPE at least 45 days from completion of the 1:1 post probe education call date. Palmetto GBA offers education at any time for providers. Providers do not have to be identified for TPE to request education.
References
- CMS Targeted Probe and Educate (TPE) web page
- Change Request 10249 (PDF, 241.88 KB)