Hospice Coalition Questions and Answers: June 9, 2022
To: Hospice Coalition Members
From: Palmetto GBA Provider Outreach and Education (POE)
Date: June 9, 2022
Location: Teleconference
Time: 12:30 p.m. ET
Attachments A and A2: Hospice Appeals Report (PDF)
Attachment B: Hospice CAP Updates (PDF)
Questions for Response
Billing Questions
1. Question: The Medicare Claims Processing Manual at 20.2.1, discusses Hospice Discharges. When addressing a patient receiving care in a non-contract facility for a condition related or not related to the terminal illness or related conditions, CMS includes the following language: “Another example would be when a hospice patient is receiving treatment for a condition unrelated to the terminal illness or related conditions in a facility with which the hospice does not have a contract, and the hospice is unable to access the patient to provide hospice services. In this example, Medicare’s expectation is that the hospice provider would consider the amount of time the patient is in that facility and the effect on the plan of care before making a determination that discharging the patient from the hospice is appropriate.”
Can Palmetto GBA give guidance, including examples, of when it will make sense to discharge the patient from services if the patient enters a non-contracted hospital and when it would not? Can you provide guidance on how the amount of time and impact of the plan of care should factor into this decision-making?
Answer: This will have to be determined by the individual hospice by considering the amount of time the patient is in that facility, the effect on the plan of care and access to the patient. If the patient is discharged due to entering facility in which the hospice does not have a contract, this is not a revocation and the patient should not be asked to revocate. This is a discharge by the hospice.
If the patient enters a non-contract facility for a condition related to the terminal illness or related conditions, the hospice may discharge the patient so the facility may receive reimbursement for the medically necessary services they provide. If no discharge occurs, the facility may seek payment from the hospice if their services are denied.
For a patient that enters a non-contract facility for a condition that is not related to the terminal illness or related conditions, the difficult question will be determining that a patient would receiving care for a condition that is not related to the terminal illness or related conditions. Unrelated services to the patient’s terminal illness and related conditions are exceptional and unusual.
2. Question: A hospice conducted an internal retrospective review of the medical record for a patient who was on service from January 4 to May 24 when the patient died. Documentation for April does not support the patient’s eligibility. The hospice interdisciplinary team and the hospice medical director strongly believe the patient was hospice eligible. And this is evidenced by the patient dying within 6 months of admission.
a. Question: What action should the hospice take? Should they cancel the claim for April?
Answer: If the hospice determines the documentation for April does not support the patient’s eligibility, the hospice shall report these non-covered days on the claim with an occurrence span code 77. A claim in the middle of a sequence of a continuous hospice election cannot be cancelled. All claims after the claim that would be cancelled would need to be cancelled also.
b. Question: Should the hospice go back to admission and cancel the claims?
Answer: This will have to be determined by the individual hospice if eligibility was or wasn’t met.
c. Question: Should the hospice go forward and cancel the claims?
Answer: This will have to be determined by the individual hospice if eligibility was or wasn’t met.
d. Question: If the patient had not died, was on service until November, and then was discharged alive for no longer being eligible, does that change the answers to a–c?
Answer: No.
3. Question: We have a handful of patients who have active Value-Based Insurance Design (VBID) coverage, but Palmetto GBA paid the claim. The patient admitted to hospice in 2022 and the Medicare Advantage (MA) Contract and Plan number is listed on the 2022 VBID payer listing. We tried to submit an 817 with code D9 and comments directing Palmetto GBA to recoup their payment due to the patient having active VBID coverage but the claim was just repaid.
a. Question: What actions should providers take to resolve? Is this a problem on Palmetto GBA’s end, or the VBID payer not reporting VBID coverage to Palmetto GBA correctly?
Answer: Palmetto GBA processes claims by the VBID MAO (MA Organization) enrollment information loaded on the CWF. If the MAO information is not correct in CWF, the MAC would pay the claim. If the MAO is loaded correctly, the claim would reject with Reason Code U523A (Narrative: The dates of service are during both a hospice election period and a MA plan's period that is in a VBID Model)
Hospices seeing this issue should reach out to the VBID Model Team with any questions, comments, or concerns about the Hospice Benefit Component at VBID@cms.hhs.gov. Palmetto GBA has sent this question to this email address and is awaiting a response.
b. Question: Should these overpayments be listed on our Quarterly Credit Balance reports?
Answer: No. When the CWF record is corrected, the claims should be adjusted and rejected, taking back the payment. System issue should never be reported on CBRs.
How the MAC will process informational Notice of Elections (NOEs) and claims:
- NOE processes and approves like normal (PB9997 location)
- A hospice would not know a patient is in a VBID MAO with the processing of the NOE
- The NOE will open the election in Medicare’s eligibility systems, same as a patient in Original Medicare
- Claims will reject with Reason Code (RC) U523A
- RC Narrative: The dates of service are during both a hospice election period and a MA plan's period that is in a VBID Model
- The rejected claims will open benefit periods in Medicare’s eligibility systems
- Therefore, if a patient leaves the MAO plan, returns to Original Medicare and continues the hospice election, they will continue from the current period on Medicare’s eligibility systems. The hospice would continue to bill the MAC and the MAC would issue payment, assuming the patient’s MAO plan has a termination date on Medicare’s eligibility systems for the dates of service billed. The MAC would not pay if Medicare’s eligibility systems were not updated to show the termination. The patient or hospice would have to contact the MAO to submit the termination.
- Therefore, if a patient leaves the MAO plan, returns to Original Medicare and continues the hospice election, they will continue from the current period on Medicare’s eligibility systems. The hospice would continue to bill the MAC and the MAC would issue payment, assuming the patient’s MAO plan has a termination date on Medicare’s eligibility systems for the dates of service billed. The MAC would not pay if Medicare’s eligibility systems were not updated to show the termination. The patient or hospice would have to contact the MAO to submit the termination.
4. Question: DCE – We’ve received many claims with reduced payment labeled with CO-132 (Demonstration Project).
a. Question: How is a provider able to identify which demonstration project applies? Are demonstration projects based on patient’s enrollment, physician’s enrollment, hospice’s enrollment?
Answer: Hospices, like other providers, elected to part of the Global and Professional Direct Contracting (GPDC) Model and should have contact information. Demonstration projects are usually based on each provider’s enrollment. Palmetto GBA does oversee or enter payment adjustments for these models.
b. Question: Is there anything in the eligibility system that indicates the patient’s demonstration project enrollment?
Answer: Please contact the model. When they were Accountable Care Organizations (ACOs), there were private entities offering eligibility system that looked up ACO enrollment.
c. Question: How can we confirm that the CO-132 payment reduction is accurate?
Answer: Please contact the model.
Medical Review Questions
5. Question: Please provide an update on the General Inpatient Care (GIP) greater than or equal to 7 days Targeted Probe and Educate (TPE) edit.
a. Question: What trends in the outcomes are you seeing thus far?
Answer:
Here are the top findings:
1. Medical Necessity is not being substantiated and supported. Hospices are sending in entire hospital records but nothing significant to support a GIP level of care.
a. Missing Medication Administration Records (MAR) is the most frequently requested documentation.
2. The physician narrative statement is not valid or present
a. Diagnosis is listed, but no overall picture of the beneficiary’s need for GIP is present.
3. The Hospice Election Statement is invalid.
a. Missing information about the Beneficiary and Family Centered Care Quality Improvement Organization (BFCC-QIO), including the right to immediate advocacy and BFCC-QIO contact information
b. Missing the notification of the individual’s (or representative’s) right to receive an election statement addendum.
c. Missing the name of the hospice on the election statement.
4. The plan of care (POC) is missing hospice interdisciplinary group (IDG) notes or the physician signature.
a. This is most frequently requested documentation about the POC.
5. Certification is missing for dates of service reviewed or is invalid:
a. Missing prognosis statement for verbal certifications.
Chapter 9 — Coverage of Hospice Services Under Hospital Insurance (PDF)
20.1 — Timing and Content of Certification
(Rev. 246, Issued: 09/14/2018, Effective: 12/17/2018, Implementation: 12/17/2018)
For the first 90-day period of hospice coverage, the hospice must obtain, no later than 2 calendar days after hospice care is initiated, (that is, by the end of the third day), oral or written certification of the terminal illness by the medical director of the hospice or the physician member of the hospice IDG, and the individual’s attending physician if the individual has an attending physician
For the subsequent periods, recertifications may be completed up to 15 days before the next benefit period begins. For subsequent periods, the hospice must obtain, no later than 2 calendar days after the first day of each period, a written certification statement from the medical director of the hospice or the physician member of the hospice’s IDG. If the hospice cannot obtain written certification within 2 calendar days, it must obtain oral certification within 2 calendar days. When making an oral certification, the certifying physician(s) should state that the patient is terminally ill, with a prognosis of 6 months or less.
b. Question: In terms of initial review and identification of providers involved in the TPE, how far along is this TPE process?
Answer: As a MAC, we focus on providers and suppliers who have among the highest claim error rates, or billing practices that vary significantly from their peers. As TPE is the selected review approach of CMS, Palmetto GBA will continue to identify providers for TPE; identification and probes are cyclical.
c. Question: What is the average denial rate?
Answer: The average charge denial rate is 16 percent and the average claim denial rate is 20 percent. The threshold for both rates is 20 percent and both rates are used to determine if a provider is removed from TPE or if they move on to the next round.
d. Question: How many or what percentage of providers will progress to Round 2?
Answer: Palmetto GBA has changed our practice in providing statistics related to individual provider performance. Palmetto GBA is focusing on problem specific data, which helps the overall provider community. Previously data posted in our articles identified how many providers were advancing to subsequent probes, along with denial reasons associated with providers that finished their probes. Our new articles are focused on how we can help providers avoid denials. One way to do this is to provide data related to all reviews conducted over an identified timeframe. Data posted reflects the results of all provider claims reviewed (completed/pending).
6. Question: We are seeing denials related to certifications. The denial reason indicates the verbal (oral) certification is missing the 6 months statement or other components. We know what constitutes a valid written certification and physician narrative because those are clearly outlined in 42 CFR 418.22.
Under section 418.22 (d), Maintenance of records, it states the Hospice staff must – (1) Make an appropriate entry in the patient's medical record as soon as they receive an oral certification; and (2) File written certifications in the medical record.
What constitutes an “appropriate entry” for a verbal (oral) certification, and more specifically, where is this outlined in the regulation or Medicare policy?
Answer: § 418.22 Certification of terminal illness
(a) Timing of certification
(1) General rule. The hospice must obtain written certification of terminal illness for each of the periods listed in § 418.21, even if a single election continues in effect for an unlimited number of periods, as provided in § 418.24(c).
(2) Basic requirement. Except as provided in paragraph (a)(3) of this section, the hospice must obtain the written certification before it submits a claim for payment.
(3) Exceptions.
(i) If the hospice cannot obtain the written certification within 2 calendar days, after a period begins, it must obtain an oral certification within 2 calendar days and the written certification before it submits a claim for payment.
(ii) Certifications may be completed no more than 15 calendar days prior to the effective date of election.
(iii) Recertifications may be completed no more than 15 calendar days prior to the start of the subsequent benefit period.
(4) Face-to-face encounter
(i) As of January 1, 2011, a hospice physician or hospice nurse practitioner must have a face-to-face encounter with each hospice patient whose total stay across all hospices is anticipated to reach the 3rd benefit period. The face-to-face encounter must occur prior to, but no more than 30 calendar days prior to, the 3rd benefit period recertification, and every benefit period recertification thereafter, to gather clinical findings to determine continued eligibility for hospice care.
(ii) During a Public Health Emergency, as defined in § 400.200 of this chapter, if the face-to-face encounter conducted by a hospice physician or hospice nurse practitioner is for the sole purpose of hospice recertification, such encounter may occur via a telecommunications technology and is considered an administrative expense. Telecommunications technology means the use of interactive multimedia communications equipment that includes, at a minimum, the use of audio and video equipment permitting two-way, real-time interactive communication between the patient and the distant site hospice physician or hospice nurse practitioner.
(b) Content of certification. Certification will be based on the physician's or medical director's clinical judgment regarding the normal course of the individual's illness. The certification must conform to the following requirements:
(1) The certification must specify that the individual's prognosis is for a life expectancy of 6 months or less if the terminal illness runs its normal course.
(2) Clinical information and other documentation that support the medical prognosis must accompany the certification and must be filed in the medical record with the written certification as set forth in paragraph (d)(2) of this section. Initially, the clinical information may be provided verbally, and must be documented in the medical record and included as part of the hospice's eligibility assessment.
7. Question: Claim Review Determination Letters continue to be non-specific and make it difficult to know what caused the denial. For example, a letter simply stated, “The claim has been fully or partially denied as the documentation submitted indicates that the statutory/regulatory requirements for the Hospice Election Statement were not met.” The letter goes on to quote the manual in regard to what must be included in an Election Statement which is not helpful in most cases. Occasionally, such as with this situation, we were able to access Remarks in DDE and see a more specific reason (screenshot below).
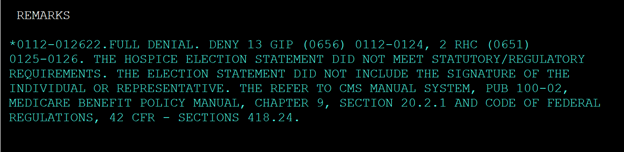
Why are the details not included in the letters? Is there an enhancement that could be made so that the Determination Letters could include the same information that is in DDE? Perhaps the same person who enters the DDE remarks can populate that information for the letters.
Answer: Letters are specific to the denial reasons provided by the Medical Review Operations team.
8. Question: What other data analysis is being completed to guide medical review audit activity?
Answer: Palmetto GBA uses local claims data from the standard claims processing systems (Fiscal Intermediary Standard System (FISS) and Multi-Carrier System (MCS)) as one of the primary sources of data used in the identification process. In addition to claims data from the standard claims processing systems, Palmetto GBA maintains CMS national data sources, as well as descriptive data for claim specific elements and identification data for beneficiaries and providers in our jurisdiction.
We use a geographic analyses through ZIP code information, which includes mapping to state and county, including population and other Census data by ZIP code and county. This enables Palmetto GBA to drill down claim comparisons within the jurisdiction, state, county. Palmetto GBA also looks at national data to help key in on problems that may not occur in our jurisdiction at the time of analysis but could have a downstream impact.
Palmetto GBA uses monthly, quarterly, semiannual, and annual utilization to help identify provider billing frequency. This helps Palmetto GBA identify if a provider can successfully complete an audit within a certain timeframe.
9. Question: Does Palmetto GBA expect/anticipate that any new medical review activity will begin in 2022. If so, what is the likely focus of the audits?
Answer: In 2022, Palmetto GBA added the New Hospice Providers and Non-Cancer Length of Stay (NCLOS) audits to the Active Medical Review List posted on our website. If new medical review audits are added, we will post the website prior to implementing.
Reference: JM Parts A, B and Home Health and Hospice Targeted Probe and Educate Active Medical Review List
General Questions
10. Question: Since the certification statement and recertification statement are not actually orders, can anyone (even non-clinicians) record the statement for the physician to sign?
Answer: Palmetto GBA does apply the CMS guidelines and regulations. We do not consider a verbal certification a verbal order.
11. Question: The NCLOS report was released in early May. Did the data show any concerning trends?
Answer: In Palmetto GBA’s jurisdiction as a whole, no concerning trends were identified. However, we have added the NCLOS audit to our active medical review list for providers who have been identified with NCLOS rates higher than their peers, within their regional area and Palmetto GBA jurisdiction.
12. Question: Medicare Benefit Policy Manual Chapter 9 states, “General inpatient care is allowed when the patient’s medical condition warrants a short-term inpatient stay for pain control or acute or chronic symptom management that cannot feasibly be provided in other settings.” Many treatments for pain control or acute or chronic symptom management can be provided in the home setting. Despite this, some terminally patients’ conditions require the inpatient setting because their condition is too severe to be controlled in the home at this time or the patient needs to stabilize with the treatment under the physician’s supervision before the patient is safe to transfer to the home-like setting. In the past, Palmetto GBA had an audit tool to guide hospices through questions they should consider when deciding if the patient qualifies for GIP as well what you expect to be in the documentation. Please offer guidance for hospices as they make these decisions.
Answer: We current provide the below resources on our website.
- Hospice GIP Audit Tool (PDF)
- Palmetto GBA GIP Video Script (PDF)
- Targeted Probe and Educate Progress Update: Hospice — GIP — General Inpatient Care
- Video Education: Hospice General Inpatient Care (GIP)
Reports
- Please provide an update on the latest quarterly appeals report.
- Please give an update on the latest cap overpayments.
Education Topics
1. Two percent Payment Adjustment (Sequestration) Changes
a. Thursday, December 16, 2021, MLN Connects
i. No payment adjustment through March 31, 2022
ii. One percent payment adjustment April 1 – June 30, 2022
iii. Two percent payment adjustment beginning July 1, 2022
2. Gap Billing Between Hospice Transfers — MLN Matters Number: MM12619 (PDF): Effective Date: July 1, 2022, a new CWF edit that no longer allows gaps of care to occur during a transfer